Peroneal Subluxation
- Home
- Conditions We Treat
- Foot & Ankle
- Peroneal Subluxation
What is Biceps Tendinopathy?
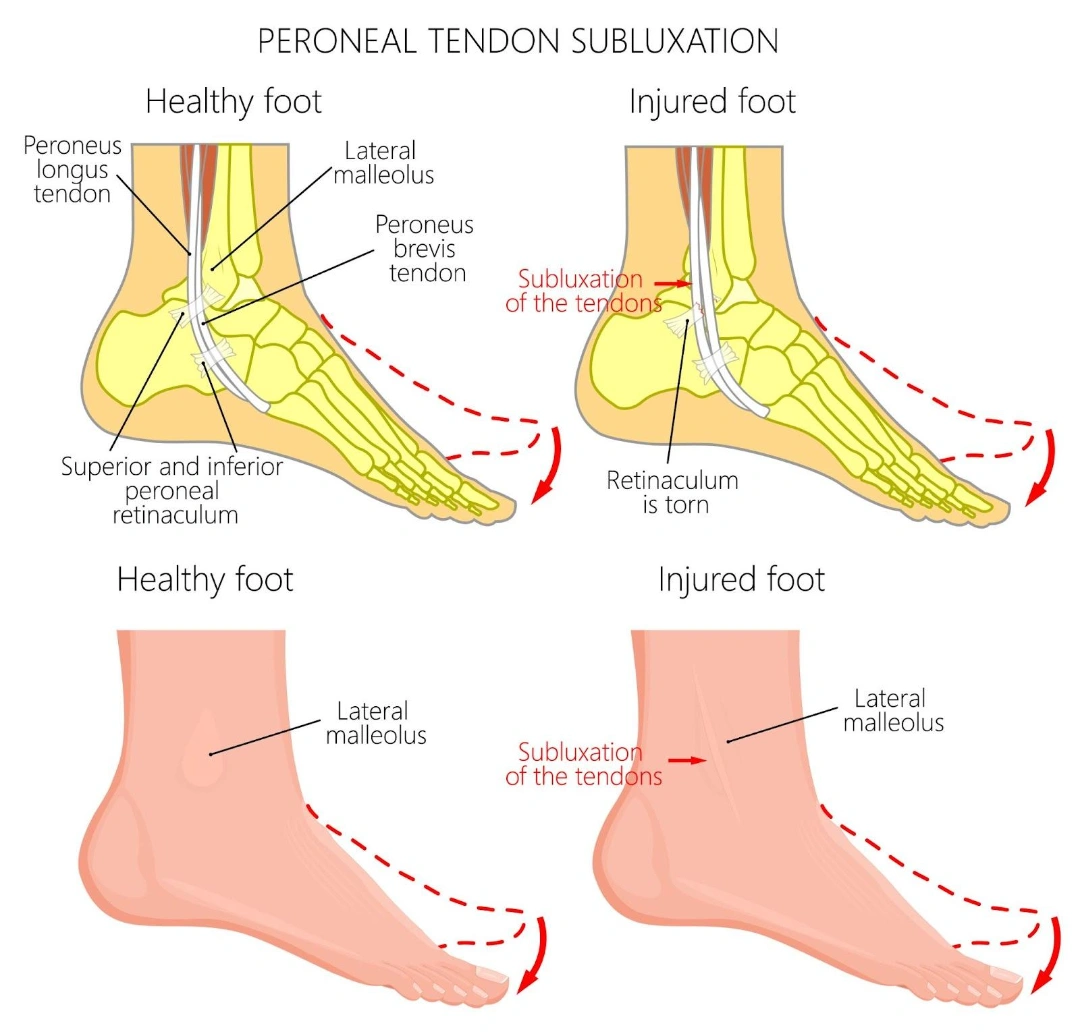
Peroneal subluxation, also known as peroneal tendon dislocation, is a rare but significant cause of pain on the outer (lateral) side of the ankle. It occurs when the peroneal tendons, the peroneus brevis and peroneus longus, slip out of their normal position behind the fibula due to damage to the superior peroneal retinaculum (SPR). Although it makes up only about 0.3–0.5% of all ankle injuries, it is frequently missed or mistaken for an ankle sprain, particularly in athletes.
Left untreated, peroneal subluxation can lead to chronic ankle instability, tendon degeneration and long-term functional impairment. Understanding the condition, its symptoms and treatment options is key to preventing complications.
What is peroneal subluxation?
The superior peroneal retinaculum is a strong fibrous band that runs along the outer ankle, securing the peroneal tendons within a groove at the back of the fibula, called the retromalleolar groove. When this structure is torn, stretched, or detached, typically due to a forceful ankle movement, the tendons can slip forward over the fibula.
This displacement may be:
- Acute — occurring suddenly after trauma, often with immediate pain and swelling.
- Chronic or recurrent — developing over time, often following a previous ankle injury that healed poorly.
In some cases, the tendon may briefly sublux during movement and return to its groove, creating intermittent symptoms.
Grades of peroneal tendon dislocation
The severity of peroneal subluxation is commonly assessed using the Eckert and Davis classification, later expanded by Oden. This grading system helps determine how far the injury has progressed, from mild retinaculum elevation to more complex tendon displacement with associated bone or cartilage injury.
Understanding the grade is essential for choosing the most appropriate treatment approach and predicting recovery outcomes.
| Grade | Description |
|---|---|
| I | SPR elevated from the fibula, allowing both peroneus brevis and peroneus longus tendons to dislocate without bone injury. |
| II | Tendon dislocation caused by avulsion of fibrocartilage from the fibula, disrupting tendon stability. |
| III | Avulsion of the fibular cortex and overlying cartilage, resulting in tendon displacement and bony involvement. |
| IV | SPR detached from its posterior attachment to the calcaneus, creating severe instability of the peroneal tendons. |
What causes peroneal subluxation?
The typical injury mechanism involves a forceful upward flexion of the foot (dorsiflexion) combined with an outward turn (eversion). This movement can tear the superior peroneal retinaculum, allowing the tendons to displace from their groove.
High-risk situations include:
- Sports injuries — especially those involving sudden stops, pivots, or lateral movements, such as basketball, football, rugby, skiing, ice-skating, dancing and gymnastics.
- Falls or missteps — such as missing a step or landing awkwardly from a jump.
- Direct trauma — a blow to the outer ankle.
Contributing factors:
- Previous ankle injuries — especially untreated or misdiagnosed sprains, which can weaken the supporting structures.
- Anatomical variations — a shallow fibular groove or weak retinaculum can predispose to subluxation.
- Lax ligaments — in individuals with generalised ligament looseness.
What are the symptoms of peroneal subluxation?

Symptoms may differ between acute and chronic cases, but most patients experience a combination of pain, mechanical symptoms and instability. Recognising these signs early can help prevent the condition from becoming long-term.
- Pain along the outer ankle — usually felt behind the lateral malleolus, especially during activity or when pressing on the affected area.
- Popping or snapping sensation — often occurs during ankle movement, particularly with sports, sudden direction changes, or pivoting.
- Swelling and bruising — localised around the outer ankle, appearing soon after the injury.
- Ankle instability — a feeling that the foot may give way, especially on uneven ground or during quick movements.
- Difficulty bearing weight — pain and weakness can limit walking, running or sporting activities.
- Aching discomfort in chronic cases — may develop with prolonged walking or standing, often accompanied by reduced athletic performance.
Who is at risk of a peroneal subluxation in Singapore?
Peroneal subluxation can affect anyone, but it is more common in individuals with certain activity patterns, foot structures, or injury histories.
- Athletes in sports with rapid pivots or cuts — such as basketball, football, rugby and gymnastics, where sudden changes in direction place high stress on the ankle.
- Skiers and skaters — quick ankle rotations and forced foot positions increase the likelihood of injury.
- People with recurrent ankle sprains — previous ligament damage can weaken ankle stability, predisposing the tendons to displacement.
- Individuals with high-arched feet — this foot type alters biomechanics, placing extra strain on the peroneal tendons and their supporting structures.
How is peroneal subluxation diagnosed?
Because symptoms can mimic a severe ankle sprain, accurate diagnosis is essential to avoid delayed treatment. A complete assessment may include:
- Clinical examination — the doctor checks for tenderness, swelling and instability. You may be asked to move your ankle in specific ways to reproduce symptoms or the tendon snap.
- X-rays — to rule out fractures or bony abnormalities.
- MRI scans — particularly useful for evaluating soft tissue injuries, showing tears in the retinaculum and tendon displacement (especially with the ankle dorsiflexed).
- CT scans — give detailed views of bone structure and groove depth, important for surgical planning.
- Dynamic ultrasound — a highly sensitive, real-time method to visualise tendon movement during ankle motion, making it ideal for detecting intermittent subluxations.
What are the treatment options for peroneal subluxation in Singapore?
Management of the condition depends on whether the injury is acute, chronic or recurrent, as well as the patient’s activity level and response to early interventions. Treatment generally falls into two categories; non-surgical options for recent injuries and surgical procedures for persistent or severe cases.
- Non-surgical management
This is mostly recommended for acute injuries where the tendon and retinaculum have a chance to heal without surgery.
- Immobilisation — use of a cast, walking boot, or ankle taping for 4–6 weeks to keep the tendon in place and allow tissue healing.
- Rest and activity modification — avoiding sports, high-impact movements and prolonged weight-bearing until the ankle regains stability.
- Pain and swelling control — applying ice, elevating the ankle and using anti-inflammatory medication to reduce discomfort and inflammation.
- Rehabilitation — structured physiotherapy to improve strength, proprioception and balance, ensuring the ankle can tolerate normal and sport-specific movements.
Note: Outcomes from conservative treatment can be unpredictable, particularly for competitive athletes, with many cases eventually requiring surgical repair.
2. Surgical management
Surgical treatment is recommended for chronic peroneal subluxation, recurrent tendon dislocations, or acute injuries that do not respond to conservative measures. The aim is to restore tendon stability, repair damaged structures and prevent future displacement. Several procedures may be used, either alone or in combination, depending on the extent of injury and anatomical factors.
- SPR repair or reattachment — this procedure involves re-securing the superior peroneal retinaculum to its original attachment on the fibula. The surgeon may use sutures, anchors, or small bone tunnels to fix the tissue back in place. Repairing the SPR restores the tendon’s primary restraint, which reduces the likelihood of future subluxation..
- Groove-deepening procedure — in patients with a naturally shallow or flat fibular groove, the surgeon reshapes and deepens the groove at the back of the fibula to better contain the tendons. This may be done with specialised burrs or chisels. By creating a deeper track, the tendons are less likely to slip forward during ankle movement..
- Tenoplasty — this refers to the repair or reconstruction of the peroneal tendons themselves if they are torn, frayed, or degenerated. Techniques may include direct suturing, tendon grafting, or tendon transfer from another site. Tenoplasty is often performed alongside SPR repair to restore both tendon structure and stability.
- Bone-block procedure — in this technique, a small bone graft is positioned on the outer lip of the fibular groove to act as a physical barrier preventing tendon displacement. This method is less common but can be effective in severe instability, especially when other anatomical features make tendon containment difficult.
3. Recovery and prognosis
Recovery time varies depending on the severity of the injury and the type of treatment performed, but most patients achieve good long-term outcomes with appropriate care.
- Post-surgery — typically involves 2 weeks in a cast, followed by 4 weeks in a walking boot to protect the repair.
- Physiotherapy — starts after immobilisation, focusing on restoring range of motion, strength, and ankle stability.
- Return to sport — generally possible within 3–4 months, though athletes in high-impact or pivot-heavy sports may require longer rehabilitation.
With correct diagnosis and treatment, most patients regain full ankle stability, although some chronic cases may experience mild residual stiffness or occasional discomfort.
Summary
Peroneal Subluxation, also known as peroneal tendon dislocation, is an uncommon but often overlooked cause of pain and instability on the outer side of the ankle. It occurs when the peroneal tendons slip out of their normal position behind the fibula, usually due to damage to the superior peroneal retinaculum. The condition may result from acute trauma or develop over time following an untreated ankle injury and is most often seen in athletes or individuals with anatomical predispositions.
Symptoms can include pain, swelling, a popping sensation and difficulty bearing weight, while diagnosis typically involves clinical assessment supported by imaging such as MRI or dynamic ultrasound. Treatment may be non-surgical in recent injuries, but chronic or recurrent cases often require surgical repair to restore stability and prevent further tendon damage. Recovery involves a structured rehabilitation programme to regain strength, stability and function.
If you are experiencing persistent ankle pain, instability or a snapping sensation, schedule a consultation with Cove Orthopaedics for a comprehensive diagnosis and tailored treatment plan to restore your mobility and prevent long-term complications.
Conditions We Treat





Frequently asked questions
Can peroneal subluxation heal on its own?
In most adults, peroneal subluxation does not resolve without targeted treatment. While symptoms may temporarily subside with rest, the underlying tendon instability often persists, increasing the risk of chronic pain, tendon damage and repeated dislocation.
What is the recurrence risk of peroneal subluxation after surgery?
Although surgical repair significantly improves stability, recurrence can occur if the repaired tissue stretches, healing is incomplete, or the ankle is reinjured. Proper rehabilitation and adherence to post-operative precautions help minimise this risk.
What complications might arise from surgical treatment of peroneal subluxation?
Potential complications include sural nerve irritation or injury, which may cause numbness or tingling along the outside of the foot, as well as general surgical risks such as infection, wound healing issues, or bleeding. In rare cases, stiffness or persistent discomfort may develop.
How effective is dynamic ultrasound in diagnosing peroneal subluxation?
Dynamic ultrasound is highly sensitive and allows real-time assessment of tendon movement, which makes it particularly effective for detecting intermittent subluxation that may be missed on MRI. It is especially useful when performed while the ankle is moved into positions that provoke symptoms.
What role does groove anatomy play in peroneal subluxation?
The shape of the retromalleolar groove behind the fibula is an important factor in tendon stability. A shallow, flat, or convex groove provides less containment for the tendons, increasing the likelihood of displacement during ankle movement.
Can peroneal subluxation occur without tearing the retinaculum?
Yes. In some cases, called intrasheath subluxation, the peroneal tendons shift within their sheath without a complete tear of the superior peroneal retinaculum. This can still cause pain, snapping and instability, and may require similar treatment.
Is peroneal subluxation common in non-athletes?
While athletes are at higher risk due to repetitive ankle stress, non-athletes can also develop peroneal subluxation. Factors such as previous ankle injuries, foot shape variations and general ligament laxity can predispose anyone to this condition.
What non-surgical measures help manage peroneal subluxation?
For select acute cases, treatment may include ankle immobilisation with a boot or cast, activity modification, supportive bracing or taping and physiotherapy focused on strengthening, balance and proprioception to improve tendon stability.
How does a previous ankle sprain relate to future peroneal subluxation?
Ankle sprains can overstretch or partially tear the retinaculum, weakening the structures that hold the tendons in place. Without full recovery, this instability can later develop into peroneal subluxation, even with minor twists or activity.



