Osteitis
Pubis
- Home
- Conditions We Treat
- Hip
- Osteitis Pubis
What is Osteitis Pubis?
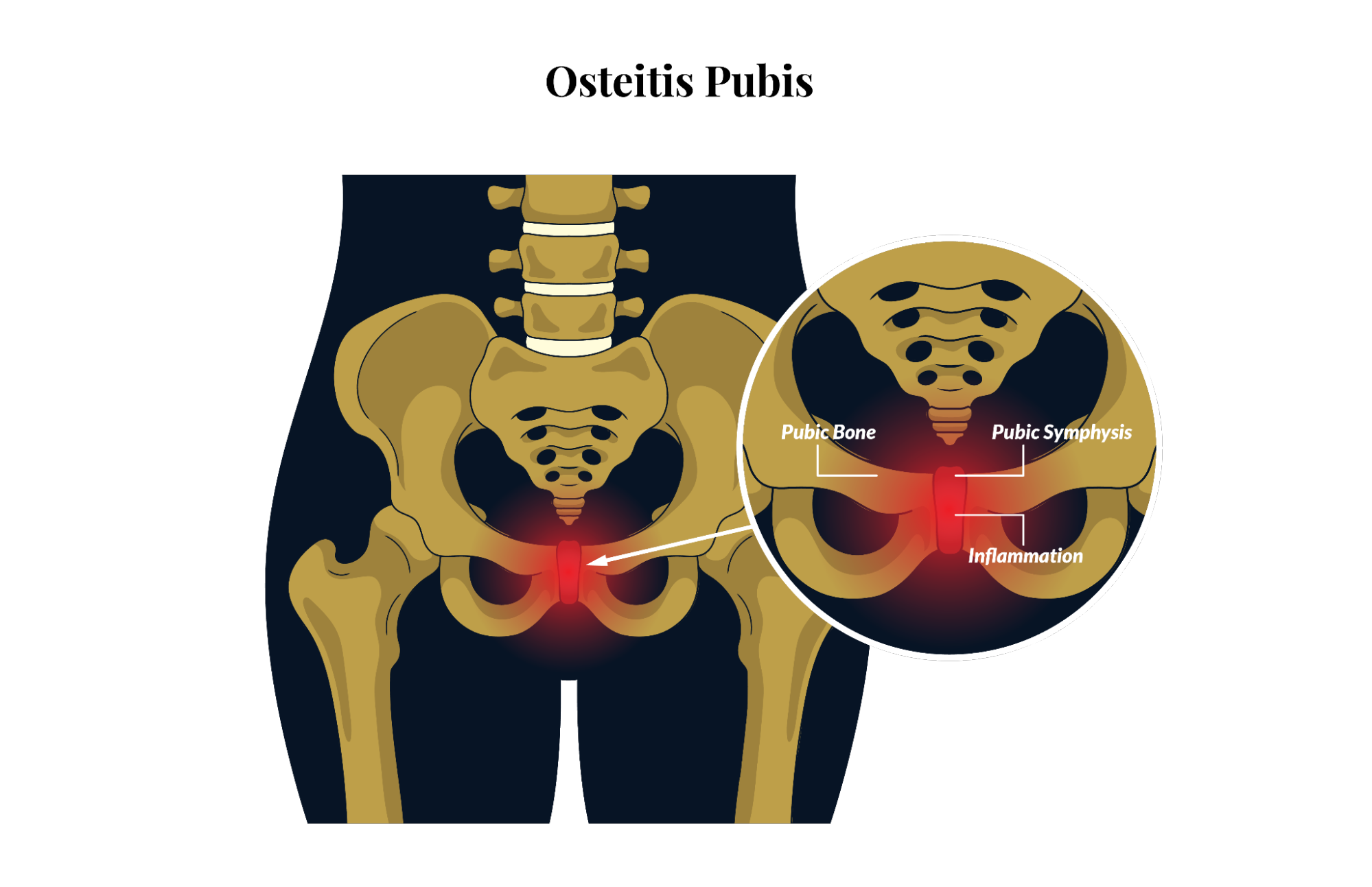
Osteitis pubis is an inflammatory condition affecting the pubic symphysis, the joint at the front of the pelvis where the two pubic bones meet. It occurs due to repetitive stress or trauma, leading to inflammation, pain, and dysfunction in the surrounding muscles, and ligaments.
This condition is commonly seen in athletes, particularly those involved in high-impact sports or activities requiring frequent twisting, kicking or rapid directional changes. While osteitis pubis is often associated with sports-related injuries, it can also develop due to pelvic surgeries, pregnancy or prolonged mechanical strain on the pelvic region.
Stages of Osteitis Pubis
Osteitis pubis is generally classified into three stages, which are:
- Acute (early onset)
- Subacute (progressive)
- Chronic (advanced)
Each stage reflects increasing severity of inflammation, and symptoms in the pubic symphysis, ranging from mild discomfort that may ease with movement to persistent, debilitating pain that interferes with daily activities.
How does Osteitis Pubis affect the body?
Osteitis pubis primarily affects the stability, and function of the pelvis. The pelvis plays a crucial role in movement, and weight-bearing activities. As such, the inflammation of the pubic symphysis disrupts normal biomechanics, leading to:
- Difficulty with weight-bearing activities, such as walking, running or climbing stairs.
- Pain, and tenderness in the lower abdomen, groin or inner thighs.
- Restricted hip mobility due to pain, and stiffness.
- Weakness or instability in the core and lower limbs, increasing the risk of further musculoskeletal issues.
In severe cases, the condition can interfere with normal gait patterns, resulting in compensatory movements that may contribute to secondary injuries in the hips, lower back or knees.
What causes Osteitis Pubis?
Osteitis pubis develops when excessive or repetitive stress is placed on the pubic symphysis, leading to inflammation, and microtears in the surrounding soft tissues. Some of the common causes include:
- Biomechanical imbalances – poor posture, weak core muscles or leg length discrepancies can place uneven stress on the pelvis.
- Overuse injuries – this is common in athletes who engage in sports like football, running or weightlifting. This is because these sports involve frequent pelvic stress.
- Pelvic surgery – procedures such as hernia repair, prostate surgery or C-sections may alter the stability of the pubic symphysis.
- Pregnancy and childbirth – hormonal changes, and increased pelvic strain during pregnancy can contribute to joint instability.
- Sudden trauma – direct impact injuries or falls on the pelvis can trigger inflammation.

What are the symptoms of Osteitis Pubis?
The symptoms of osteitis pubis typically develop gradually and may worsen over time. Common symptoms include:
- A deep, aching discomfort in the groin or lower abdomen that intensifies with movement
- Changes in the way you walk
- Clicking or popping sensations in the pelvis when moving
- Hip and thigh stiffness
- Pain during physical activity
- Swelling around the pelvic region
- Tenderness over the pubic bone
Who is at risk of Osteitis Pubis?
Although osteitis pubis is relatively uncommon, certain individuals are more prone to developing the condition. These include:
- Athletes and physically active individuals – those involved in high-impact sports, such as football, rugby, running or weightlifting, are at greater risk due to repetitive stress on the pubic symphysis.
- Individuals with biomechanical imbalances – poor posture, leg length discrepancies or misalignment of the pelvis can contribute to abnormal stress distribution, increasing the likelihood of developing osteitis pubis.
- Post-surgical patients – individuals who have undergone pelvic, abdominal or urological surgeries may experience altered biomechanics or scar tissue formation, contributing to pubic symphysis inflammation.
- Pregnant and postpartum women – hormonal changes and increased pelvic laxity during pregnancy, combined with the physical strain of childbirth, can place excessive stress on the pubic symphysis.
- People with repetitive strain occupations – jobs that involve frequent squatting, lifting or sudden directional changes can lead to overuse injuries in the pelvic region.
Those with a history of pelvic trauma – previous fractures, falls or direct impact to the pelvic area may predispose individuals to chronic inflammation, and irritation of the pubic symphysis.
How is Osteitis Pubis diagnosed?
Diagnosing osteitis pubis requires a comprehensive evaluation to confirm the condition, and rule out other potential causes of pelvic pain. Some of the potential causes include adductor tendinopathy, and Sportsman’s groin.
Physical Examination
Our orthopaedic specialist will perform various assessments to identify the source of pain, and evaluate the severity of the condition. This includes:
- Functional movement assessment – analysing walking, running or specific movements helps identify gait abnormalities or biomechanical issues contributing to pelvic strain.
- Palpation of the pubic symphysis – the specialist will apply pressure to the pubic symphysis to check for tenderness, swelling or instability.
- Range of motion tests – the patient may be asked to perform movements such as hip flexion, abduction or adduction to assess pain levels, and mobility restrictions.
How is Osteitis Pubis diagnosed?
On top of physical examination, our orthopaedic specialist may recommend imaging tests to be done. This is to confirm the diagnosis, and assess the extent of inflammation or damage.
- Magnetic Resonance Imaging (MRI) – MRI scans provide detailed images of the pubic symphysis, surrounding soft tissues, and any structural abnormalities. It is often used to detect chronic inflammation or tendon involvement.
- Ultrasound – a real-time ultrasound scan may be used to assess soft tissue inflammation, and guide treatment decisions.
- X-rays – while X-rays do not show soft tissues, they can help rule out bone-related issues such as fractures or osteoarthritis.
How is Osteitis Pubis treated in Singapore?
Treating osteitis pubis is highly dependent on the severity of the condition. Our orthopaedic specialist tailors a personalised treatment plan to promote healing, and prevent recurrence.

Conservative Treatments
- Bracing or supportive taping – in some cases, kinesiology tape or pelvic support braces may be recommended to reduce strain, and provide additional stability.
- Ice therapy – applying ice packs to the affected area for 15 – 20 minutes several times a day can help reduce pain, and inflammation.
- Medications – non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed for pain, and inflammation management, though they should be used with caution to avoid masking symptoms.
- Rest and activity modification – avoiding high-impact activities such as running, jumping or heavy lifting reduces strain on the pubic symphysis, and allows inflammation to subside.
- Shockwave therapy – extracorporeal shockwave therapy (ESWT) may be used to stimulate healing by increasing blood flow, and promoting tissue regeneration.
Injection Therapy
- Platelet-Rich Plasma (PRP) therapy – PRP injections use the patient’s own platelets to promote tissue repair, and accelerate healing.
- Corticosteroid injections – while corticosteroid injections can provide temporary pain relief, they are used sparingly as they may weaken soft tissues over time.
Rehabilitation and Recovery
- Biomechanical assessment – addressing movement issues, such as poor posture or running form, helps prevent future strain on the pelvic region.
- Gradual return to activity – patients are guided through a progressive rehabilitation plan, starting with gentle mobility exercises before resuming normal activities.
- Long-term strength training – strengthening the core, hip, and pelvic muscles reduces the risk of reinjury and improves overall stability.
- Physical therapy – a structured rehabilitation programme is essential for recovery. This includes:
- Strengthening exercises to improve core and pelvic stability, reducing stress on the pubic symphysis.
- Stretching routines to enhance hip and groin flexibility, preventing muscle tightness that can exacerbate symptoms.
- Gait retraining to correct movement patterns that may contribute to excessive pelvic stress.
Surgical Treatments
Surgery is typically considered only in severe or persistent cases of osteitis pubis that do not respond to conservative treatments. The goal of surgical intervention is to alleviate pain, restore stability, and promote proper healing of the pubic symphysis.
Debridement Surgery
Debridement surgery involves the removal of inflamed or damaged soft tissue around the pubic symphysis to promote healing, and reduce chronic pain. Over time, excessive stress on the pubic symphysis can lead to the accumulation of degenerated tissue, fibrosis, and persistent inflammation, which may impair natural healing.
- During the procedure, the surgeon carefully removes inflamed or necrotic tissue while preserving as much healthy tissue as possible.
- In some cases, small portions of overgrown bone (osteophytes) may also be shaved down to reduce irritation, and improve joint function.
- This procedure is usually performed using minimally invasive techniques to reduce post-surgical discomfort, and speed up recovery.
Stabilisation Procedures
In cases where osteitis pubis has led to significant instability of the pubic symphysis, surgical stabilisation may be required to restore proper function. Chronic inflammation, and microtears can weaken the connective tissues, and ligaments supporting the pubic symphysis, leading to excessive movement in the joint, ongoing pain, and impaired mobility.
Stabilisation procedures may involve:
- Pubic symphysis fixation – the surgeon may use metal plates, screws or a combination of fixation devices to stabilise the joint, and limit abnormal movement.
- Bone grafting – in cases of severe degeneration, bone grafts may be used to reinforce the pubic symphysis, and promote long-term joint stability.
- Ligament repair or reconstruction – if the ligaments surrounding the pubic symphysis have been significantly damaged, they may be repaired or reconstructed using sutures or graft materials.
Summary

Living with osteitis pubis can be frustrating, especially when it interferes with daily activities, and the sports you love. The pain, and stiffness can make even simple movements feel challenging, but the good news is that with the right approach, recovery is possible. Early diagnosis and a well-structured treatment plan can help prevent long-term issues and get you back to moving comfortably.
Schedule an appointment with us today for a comprehensive assessment and a personalised treatment plan designed to get you back to pain-free movement.
Frequently asked questions
Which sports carry a higher risk of developing osteitis pubis?
Sports that involve repetitive running, kicking, twisting or sudden directional changes place individuals at a higher risk of osteitis pubis. These include football, rugby, hockey, long-distance running, and ballet. Athletes in these sports frequently strain the pelvic region, leading to inflammation in the pubic symphysis.
Can osteitis pubis be mistaken for another condition?
Yes, osteitis pubis shares symptoms with several other conditions, such as hip labral tears, adductor tendinopathy, sports hernias, and sacroiliac joint dysfunction. Due to the overlap in symptoms, an accurate diagnosis by a medical professional is essential to ensure appropriate treatment.
How long does recovery from osteitis pubis take?
Recovery time varies depending on the severity of the condition, and adherence to treatment. Mild cases may resolve within a few weeks with rest and physiotherapy, while more severe cases can take several months. In chronic cases, rehabilitation may extend beyond six months, and surgical intervention is rarely required.
Can osteitis pubis be prevented?
While osteitis pubis cannot always be entirely prevented, reducing risk factors is possible. Maintaining proper conditioning, strengthening core, and pelvic muscles, incorporating flexibility exercises, and gradually increasing training intensity can help minimise strain on the pubic symphysis. Additionally, proper warm-ups, cooldowns, and addressing biomechanical imbalances also play a crucial role in prevention.
Can osteitis pubis recur after treatment?
Yes, recurrence is possible, particularly if an individual returns to high-impact activities too soon or does not fully address underlying risk factors such as muscle imbalances or poor biomechanics. A structured rehabilitation programme, and ongoing preventive measures can significantly lower the likelihood of recurrence.
Why should I see an orthopaedic specialist instead of a chiropractor?
An orthopaedic specialist is trained to diagnose, and manage musculoskeletal conditions, including osteitis pubis, with evidence-based treatments such as physiotherapy, anti-inflammatory medications, and, in severe cases, surgical options.
While chiropractors focus on spinal adjustments, and musculoskeletal manipulation, they may not provide the comprehensive care required for conditions affecting the pubic symphysis.



