Achilles
Tears
- Home
- Conditions We Treat
- Foot & Ankle
- Achilles Tears
What is Achilles tear?
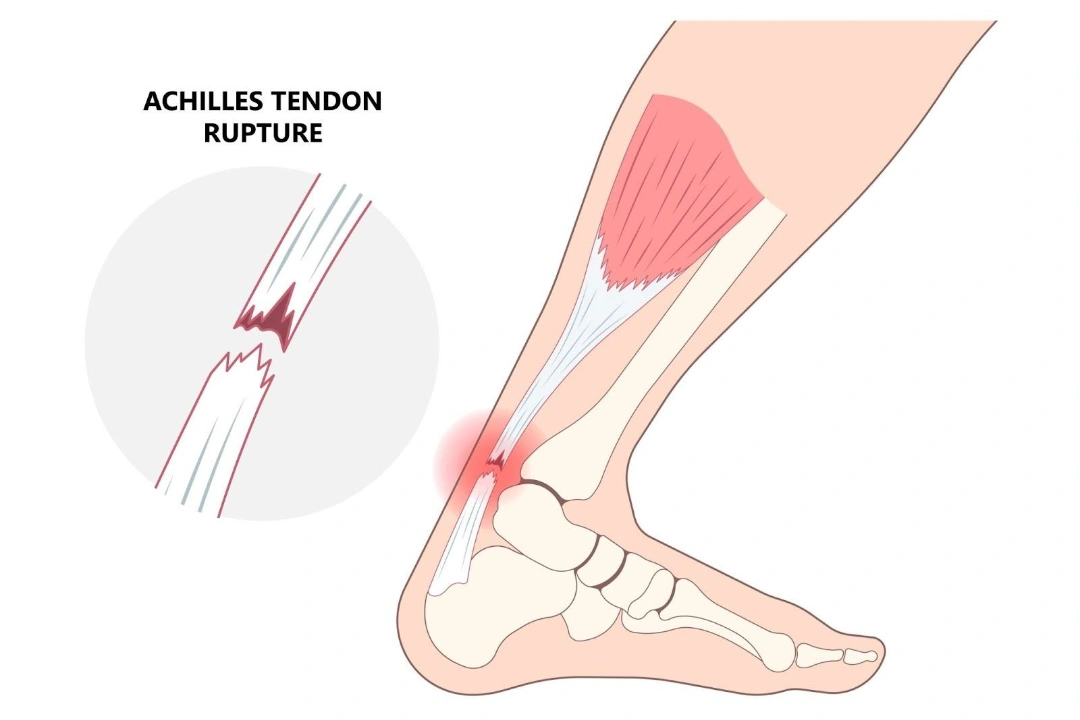
An Achilles tear refers to an injury involving a partial or complete rupture of the Achilles tendon, the thick fibrous cord that connects the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). It is the strongest and largest tendon in the human body, essential for walking, running, jumping, and pushing off the foot. When this tendon is torn, either through sudden force or chronic degeneration, it results in significant impairment of lower limb function.
Achilles tears are most commonly seen in men aged 30 to 50, particularly those who participate in recreational sports involving sudden acceleration, pivoting, or jumping, such as basketball, football, or tennis. The injury typically occurs during activities that place abrupt stress on the tendon, especially when the foot is dorsiflexed while the calf muscles are contracted.
A complete tear often presents with a sudden “pop” or snapping sensation in the back of the ankle, followed by sharp pain, swelling, and difficulty walking. Many individuals describe the feeling as being kicked or struck on the back of the leg. In contrast, partial tears may cause ongoing discomfort, weakness, and stiffness during activity, without the acute rupture symptoms.

What causes Achilles Tear?
An Achilles tear is typically caused by either a sudden forceful strain on the tendon or long-term degeneration that weakens it over time. The most common scenario involves an abrupt movement that overstretches the tendon, such as pushing off forcefully during sprinting, jumping, or changing direction, especially when the calf muscle is not properly warmed up or conditioned.
Other key causes and contributing factors include:
- Overuse and degeneration — repeated microtrauma from running or high-impact sports can lead to chronic tendinopathy, making the tendon more susceptible to tearing.
- Sudden increase in activity — rapidly intensifying your training without adequate progression can overload the tendon.
- Age-related changes — tendon elasticity and blood supply decrease with age, particularly in men over 30, increasing the risk of rupture.
- Improper footwear or training surfaces — wearing unsupportive shoes or exercising on hard or uneven surfaces can place extra stress on the Achilles.
- Use of medications — corticosteroid injections near the tendon and certain antibiotics like fluoroquinolones have been linked to increased risk of tendon rupture.
In many cases, Achilles tears occur in individuals who may not have had significant prior symptoms, especially during explosive or high-stress movements. Identifying and addressing risk factors early can help reduce the chance of injury.
What are the symptoms of an Achilles Tear?
The symptoms of an Achilles tear typically appear suddenly and are often unmistakable. In the case of a complete rupture, individuals often describe hearing or feeling a sudden “pop” or snapping sensation at the back of the lower leg, followed by sharp pain.
Common symptoms include:
- Sudden pain at the back of the ankle or calf — often described as feeling like being kicked or struck in the back of the leg.
- Swelling and bruising — rapid swelling may appear around the heel or lower calf, sometimes accompanied by bruising.
- Difficulty walking or standing on tiptoes — the inability to push off the foot, especially when climbing stairs or walking uphill, is a key sign.
- Weakness in the affected leg — a noticeable loss of strength, particularly in plantarflexion (pointing the foot downward).
- Gap in the tendon — in a full rupture, a gap may be felt along the tendon just above the heel bone.
- Stiffness or tenderness — particularly in partial tears, there may be persistent discomfort, tightness, or pain during physical activity.
In less severe or partial tears, symptoms may be more subtle and develop gradually, with recurring pain during exercise. Any persistent or sudden pain in the Achilles region warrants medical attention, as early diagnosis and treatment can significantly affect recovery outcomes.

Who is at risk of Achilles Tears in Singapore?
Achilles tears can affect anyone, but certain groups are at higher risk due to specific physical, lifestyle, or medical factors. These include:
- Men aged 30 to 50 — this group, particularly those engaged in recreational sports, is statistically more prone to tendon rupture.
- Athletes and weekend warriors — sudden bursts of activity, especially without proper conditioning or warm-up, can strain the tendon.
- People with a history of Achilles tendinopathy — chronic inflammation or degeneration weakens the tendon over time.
- Those with tight calf muscles or limited ankle flexibility — poor biomechanics can increase tendon stress.
- Individuals taking certain medications — fluoroquinolone antibiotics and corticosteroids have been associated with increased tendon vulnerability.
- People who rapidly increase their activity level — a sudden uptick in training intensity or duration can overwhelm the tendon’s capacity to adapt.
- Those wearing improper footwear — lack of heel support or cushioning during high-impact activities can contribute to injury risk.
How is an Achilles Tear diagnosed?
Diagnosing an Achilles tear usually begins with a detailed history and physical examination by an orthopaedic specialist. The goal is to determine whether the tendon is partially torn or completely ruptured.
Key diagnostic steps include:
- Patient history — the doctor will ask about the onset of symptoms, any popping sensation, pain location, and recent activities or injuries.
- Physical examination — this includes checking for swelling, bruising, tenderness, and any visible or palpable gap in the tendon above the heel.
- Thompson test — a common clinical test where the patient lies face down and the calf is squeezed. In a normal tendon, the foot should automatically point downward. Lack of movement suggests a complete tear.
- Range of motion and strength assessment — the doctor may test your ability to push off the foot or stand on tiptoes.
If the diagnosis is uncertain or to assess the extent of the injury, imaging may be recommended:
- Ultrasound — useful for detecting partial tears and assessing tendon structure in real time.
- MRI (Magnetic Resonance Imaging) — provides a detailed view of the tendon and is especially helpful in evaluating complex or chronic cases.
What are the treatment options for Achilles Tears in Singapore?
Treatment for an Achilles tear depends on whether the tendon is partially or completely torn, as well as the patient’s age, activity level, and overall health. The main goals are to restore tendon strength and function, prevent re-rupture, and enable safe return to activity.
Non-surgical treatment
Partial tears and some complete tears can be managed without surgery, particularly in less active or older individuals. Conservative treatment includes:
- Immobilisation — a walking boot or cast is used to keep the foot in a flexed position (plantarflexion) to allow the tendon to heal.
- Physiotherapy — after immobilisation, a structured rehabilitation programme helps restore strength, flexibility, and balance.
- Gradual return to activity — progressive loading of the tendon under supervision reduces re-injury risk.
Studies have shown that, with proper rehabilitation, non-surgical treatment can result in similar long-term outcomes to surgery, though there may be a slightly higher risk of re-rupture.
Surgical treatment
Surgical repair is often recommended for:
- Complete tendon ruptures in younger or active individuals
- Cases with tendon retraction or gap
- Failed conservative treatment
Surgical options include:
- Open repair — the torn ends of the tendon are stitched back together through an incision in the back of the leg.
- Minimally invasive repair — smaller incisions reduce wound complications and promote faster healing.
After surgery, the patient typically undergoes a similar rehabilitation protocol, beginning with immobilisation and progressing to physiotherapy.
Your orthopaedic specialist will help determine the most suitable approach based on the extent of the tear and your personal goals.
Summary
An Achilles tear is a serious injury involving a partial or complete rupture of the tendon that connects the calf muscles to the heel bone. It commonly affects men aged 30 to 50 and is often triggered by sudden forceful movements or gradual degeneration from overuse. Symptoms typically include sharp pain, swelling, and difficulty walking or standing on tiptoe.
Diagnosis is made through clinical examination and imaging, while treatment depends on the severity of the tear, ranging from conservative care to surgical repair. Recovery can take several months and requires structured rehabilitation.
If you are experiencing persistent pain, weakness, or suspect an Achilles tear, schedule a consultation with Cove Orthopaedics for a thorough assessment and personalised treatment plan.
Frequently asked questions
Can an Achilles tear heal by itself?
Partial Achilles tears may heal with rest, immobilisation, and physiotherapy, especially if the tendon ends remain aligned. Complete Achilles tears usually require medical or surgical intervention to restore function.
How long does recovery take for Achilles tears?
Recovery time varies depending on the severity of the Achilles tear and the treatment method. Partial tears may take 2–3 months, while complete tears often require 6–12 months for full recovery.
Is it safe to walk with Achilles tears?
Walking with Achilles tears can be difficult and is generally not advised without medical supervision. Weight-bearing may be allowed in a boot for certain partial tears but is typically restricted in complete ruptures.
What are the risks of surgery for Achilles tears?
Surgical repair of Achilles tears carries risks such as wound infection, nerve injury, scarring, or delayed healing. However, these risks are reduced with minimally invasive techniques and proper postoperative care.
How do doctors decide between surgery and non-surgical treatment for Achilles tears?
The choice depends on factors like the size of the tendon gap, patient age, physical activity level, and personal preference. Imaging and physical assessment help guide the treatment plan for Achilles tears.
Can Achilles tears happen again after healing?
Yes, re-rupture is possible, especially if rehabilitation is rushed or incomplete. Strengthening exercises, proper footwear, and gradual return to activity help lower the risk of recurrent Achilles tears.
Are Achilles tears career-ending for athletes?
Achilles tears are serious injuries, but many athletes can return to sport after surgery and rehabilitation. However, some may experience reduced performance or agility even after recovery.
What exercises are safe during recovery from Achilles tears?
Early-stage rehabilitation for Achilles tears often involves gentle range-of-motion movements, progressing to calf strengthening and balance exercises. All activities should be guided by a physiotherapist.
Conditions We Treat








