Peroneal Tendinopathy
- Home
- Conditions We Treat
- Foot & Ankle
- Peroneal Tendinopathy
Introduction
Peroneal tendinopathy is a relatively under-recognised but important cause of pain on the outer side of the ankle. It affects the peroneal tendons, two strong, cord-like structures that run along the outside of the ankle and play a critical role in stabilising the foot during walking, running, and sporting activities. When these tendons become irritated, inflamed, or damaged, it can lead to persistent discomfort, reduced ankle stability and difficulty performing everyday or athletic movements.
Because peroneal tendinopathy can mimic other ankle injuries, such as sprains, it is often misdiagnosed. This can delay appropriate treatment and increase the risk of chronic pain or long-term ankle weakness.

What is peroneal tendinopathy?
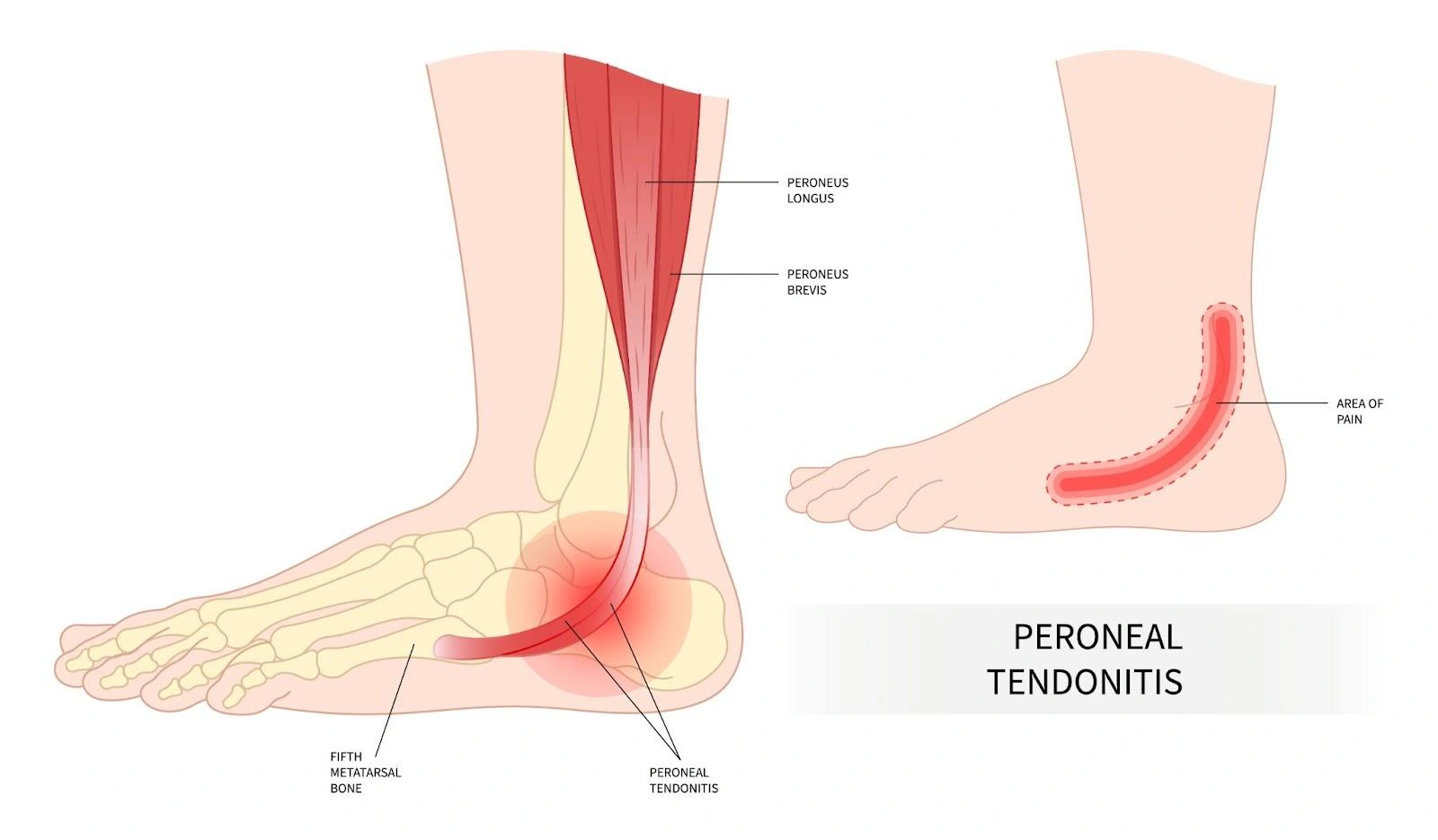
Peroneal tendinopathy is a broad term used to describe conditions that affect the peroneal tendons on the outer side of the ankle. These tendons can develop problems due to overuse, sudden injury, structural issues in the foot or ankle, or a combination of factors.
The condition can take different forms:
- Peroneal tendonitis — irritation and inflammation of the tendon, often due to repetitive overloading.
- Peroneal tendinosis — gradual degeneration and weakening of the tendon fibres, usually from long-standing strain without enough recovery.
- Peroneal tenosynovitis — inflammation of the sheath that surrounds and lubricates the tendon.
- Peroneal subluxation — partial displacement of the tendon from its normal groove behind the ankle bone, sometimes causing a noticeable “snap” or “pop” during movement.
- Tendon tears or ruptures — partial or complete disruptions in the tendon fibres, which can result from acute injury or from degeneration over time.
If not diagnosed and managed early, these problems can progress, leading to chronic instability of the ankle and even long-term loss of function.
Which tendons are involved in peroneal tendinopathy?
The peroneal tendons are part of the ankle’s complex support system and understanding their anatomy helps explain why injuries here can be so limiting.
- Peroneus brevis tendon — this tendon runs from the peroneus brevis muscle along the lower outer leg, passes behind the bony bump on the outside of the ankle (lateral malleolus) and attaches to the base of the fifth metatarsal on the outside of the foot. It helps lift the outer edge of the foot (eversion) and stabilises the ankle when standing or moving on uneven surfaces.
- Peroneus longus tendon — originating from the peroneus longus muscle, this tendon shares the same path behind the lateral malleolus before travelling under the arch of the foot to attach near the base of the first metatarsal and medial cuneiform. It assists in both ankle stability and maintaining the arch of the foot.
- Superior peroneal retinaculum (SPR) — this fibrous band secures both tendons in the retromalleolar groove behind the fibula. If the SPR is torn or stretched, the tendons can slip out of place, leading to subluxation or instability.
Because these tendons work constantly during walking, running and balance activities, they are vulnerable to both overuse injuries and acute trauma.
What causes peroneal tendinopathy?
Peroneal tendinopathy can develop from a single event or gradually over time. Several factors may contribute to its onset:
- Overuse and repetitive strain — activities involving repetitive ankle movements, such as running, jumping, or rapid direction changes, can overload the tendons, especially if training intensity increases too quickly.
- Acute injury — a sudden twist of the ankle or a forceful landing can damage the tendons directly or strain their supporting structures.
- Anatomical variations — a shallow or flat fibular groove or a low-lying peroneus brevis muscle belly can cause the tendons to rub excessively, making injury more likely.
- Chronic ankle instability — repeated ankle sprains can stretch ligaments and alter the tendons’ normal motion, increasing the risk of tendinopathy.
- Inappropriate footwear and poor technique — shoes lacking lateral support or improper movement mechanics can place extra strain on the peroneal tendons over time.
What are the symptoms of peroneal tendinopathy?
The symptoms of peroneal tendinopathy depend on the type and severity of the tendon injury, but they often develop gradually and worsen over time.
- Pain on the outer ankle — usually felt behind or below the lateral malleolus, often worsening with activity and improving with rest.
- Swelling and warmth — the area over the tendon may feel puffy and warmer than the surrounding skin.
- Tenderness on touch — pressing along the course of the tendon can reproduce pain.
- Snapping or popping sensation — common in subluxation, when the tendon shifts out of place during ankle movement.
- Ankle instability — a feeling that the ankle may “give way,” particularly when changing direction or walking on uneven ground.
- Reduced strength or endurance — activities such as climbing stairs, pushing off during running, or prolonged walking may become difficult.
Who is most at risk of peroneal tendinopathy in Singapore?
Although anyone can develop peroneal tendinopathy, certain people have a higher likelihood due to their activities, anatomy or health background:
- Athletes in high-demand sports — runners, dancers, footballers, rugby players, basketball players and skiers are particularly at risk due to repetitive ankle stress.
- Middle-aged and older adults — tendons naturally lose elasticity and strength with age, making them more vulnerable to injury.
- People with high-arched feet (pes cavus) — this foot shape increases lateral pressure on the ankle tendons.
- Those with previous ankle injuries — a history of sprains, fractures, or instability can predispose tendons to injury.
- Individuals with certain medical conditions — diabetes, gout, rheumatoid arthritis and osteoarthritis can affect tendon structure and healing capacity.
How is peroneal tendinopathy diagnosed?
Diagnosis begins with a thorough history and physical examination, followed by imaging tests if necessary:
- Clinical examination — your doctor will check for swelling, tenderness, ankle stability, and any abnormal movement of the tendons during specific motions.
- X-rays — these can rule out bone-related causes such as fractures or arthritis.
- MRI scans — provide detailed images of both tendons and their surrounding structures, showing inflammation, degeneration, or tears.
- Dynamic ultrasound — uses sound waves to visualise tendon movement in real time, making it especially useful for detecting subluxation during ankle motion.
What are the treatment options for peroneal tendinopathy in Singapore?
Treatment depends on the severity of the tendon injury, the type of problem (inflammation, degeneration, subluxation, or tear) and your lifestyle or sporting goals. The aim is to relieve pain, restore function and prevent further damage. Management falls into two main categories:
- Conservative (non-surgical) management
This is usually the first approach for mild to moderate injuries and for many inflammatory tendon conditions.
- Rest and activity modification — limiting activities that worsen pain, such as running or high-impact sports, gives the tendon time to recover. Cross-training with low-impact exercises like swimming or cycling helps maintain fitness without overloading the tendon.
- Immobilisation — a walking boot, cast, or ankle brace can be worn for several weeks to keep the tendon stable and reduce mechanical stress. In some cases, a lateral heel wedge is used inside the shoe to offload the peroneal tendons.
- Physiotherapy — rehabilitation focuses on strengthening the peroneal muscles and other stabilisers of the ankle, restoring flexibility and improving proprioception (balance and joint control). Your physiotherapist may also address biomechanical issues, such as foot posture, that contribute to tendon overload.
- Anti-inflammatory medication — non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation in cases such as peroneal tendonitis or tenosynovitis, but they are less effective for degenerative tendinosis.
- Footwear adjustments and orthotics — supportive shoes and custom orthotic inserts may correct abnormal foot mechanics, especially in those with high arches or excessive inward/outward rolling of the foot.
2. Surgical management
Surgery is recommended for persistent symptoms after months of structured conservative care, for recurrent tendon subluxation, or for significant tendon tears. Each procedure is chosen based on the type of damage and the overall health of the tendon.
- Debridement and synovectomy — this procedure removes frayed or degenerated tendon tissue along with any inflamed sheath lining. The aim is to leave behind only healthy, strong tendon fibres. Debridement is often performed when the tendon is mostly intact but has areas of damage that cause persistent pain.
- Tendon repair or tubularisation — in cases of partial tears, the damaged section of tendon is repaired by suturing the fibres together to restore its round, cord-like shape (tubularisation). This improves the tendon’s ability to glide smoothly and bear load. Tubularisation is particularly useful in “split tears” of the peroneus brevis tendon.
- Tenodesis — when a tendon is too badly damaged to repair, it can be attached to the other peroneal tendon to restore function. For example, a severely torn peroneus brevis may be anchored to the peroneus longus. This sacrifices some independent function but preserves overall ankle stability and eversion strength.
- Tendon grafting (reconstruction) — in cases of extensive tendon loss, tissue from another part of the body (autograft) or from a donor (allograft) is used to reconstruct the tendon. Grafting restores length and strength when primary repair is impossible. Autografts integrate well but involve a second surgical site, while allografts avoid donor site issues but have a longer incorporation time.
- Superior peroneal retinaculum (SPR) repair — if the SPR is torn and the tendons are subluxating, it is reattached to its original bony attachment to hold the tendons in place.
- Groove-deepening procedure — in people with a shallow or flat fibular groove, the surgeon reshapes and deepens the groove to better house the tendons, often combined with SPR repair. This reduces the chance of recurrent subluxation.
- Bone-block procedure — a small piece of bone is positioned at the edge of the fibular groove to act as a barrier, physically preventing the tendons from slipping forward. This is generally reserved for severe instability or cases where other stabilisation methods have failed.
Summary
Peroneal tendinopathy is a condition where the tendons along the outside of the ankle become irritated or overloaded, causing pain and swelling that can easily be mistaken for a simple ankle sprain. Because the injury affects the tendons rather than the ligaments, it requires a different approach to management and leaving it unchecked can lead to persistent pain or instability.
Thankfully, treatment is possible. With proper diagnosis, guided rehabilitation and supportive care, recovery is achievable and you can get back on track with your daily activities. Schedule a consultation with us today for a detailed diagnosis and personalised treatment plan.
Conditions We Treat





Frequently asked questions
Does peroneal tendinopathy show up on X-ray or MRI?
Peroneal tendinopathy may not appear on X-rays, which are mainly used to rule out bone issues. MRI can detect tendon inflammation, degeneration and tears; dynamic ultrasound is especially useful for seeing real-time tendon movement and subluxation.
How long does it take for peroneal tendinopathy to heal?
Recovery from peroneal tendinopathy generally takes several weeks with conservative treatment. Mild cases may resolve in 6–12 weeks, while chronic or severe cases, or those requiring surgery, may take several months.
Can peroneal tendinopathy lead to a tear if untreated?
Yes, untreated peroneal tendinopathy, especially when degeneration is present, can progress to a partial or complete tendon tear, increasing the risk of instability and persistent pain.
Can peroneal tendinopathy cause changes in foot posture or shape over time?
Chronic peroneal tendinopathy, particularly with degenerative tears, may alter tendon function and result in secondary foot posture changes, such as increased arch height or varus alignment.
Can peroneal tendinopathy cause nerve symptoms like tingling or numbness?
Yes, inflammation from peroneal tendinopathy can sometimes irritate nearby nerves, causing tingling, numbness, or burning sensations along the outer foot.
How likely is full recovery after surgery for peroneal tendinopathy?
Post-surgery outcomes for peroneal tendinopathy are generally good as studies report that around 85–95% of patients return to sports or previous activity levels, although surgery comes with typical risks like infection or stiffness.
Can peroneal tendinopathy develop in non-athletes?
Yes, while athletes are at higher risk, peroneal tendinopathy can affect anyone with predisposing factors such as anatomical foot variations, prior ankle injury, or chronic repetitive loading, not just formal athletic activity.
Are custom orthotics helpful for peroneal tendinopathy?
Custom orthotic inserts, especially with lateral support, can reduce tendon strain by correcting foot alignment, offering effective support in managing peroneal tendinopathy, particularly in people with high arches or varus alignment.



