Adductor Tendinopathy
What is adductor tendinopathy?
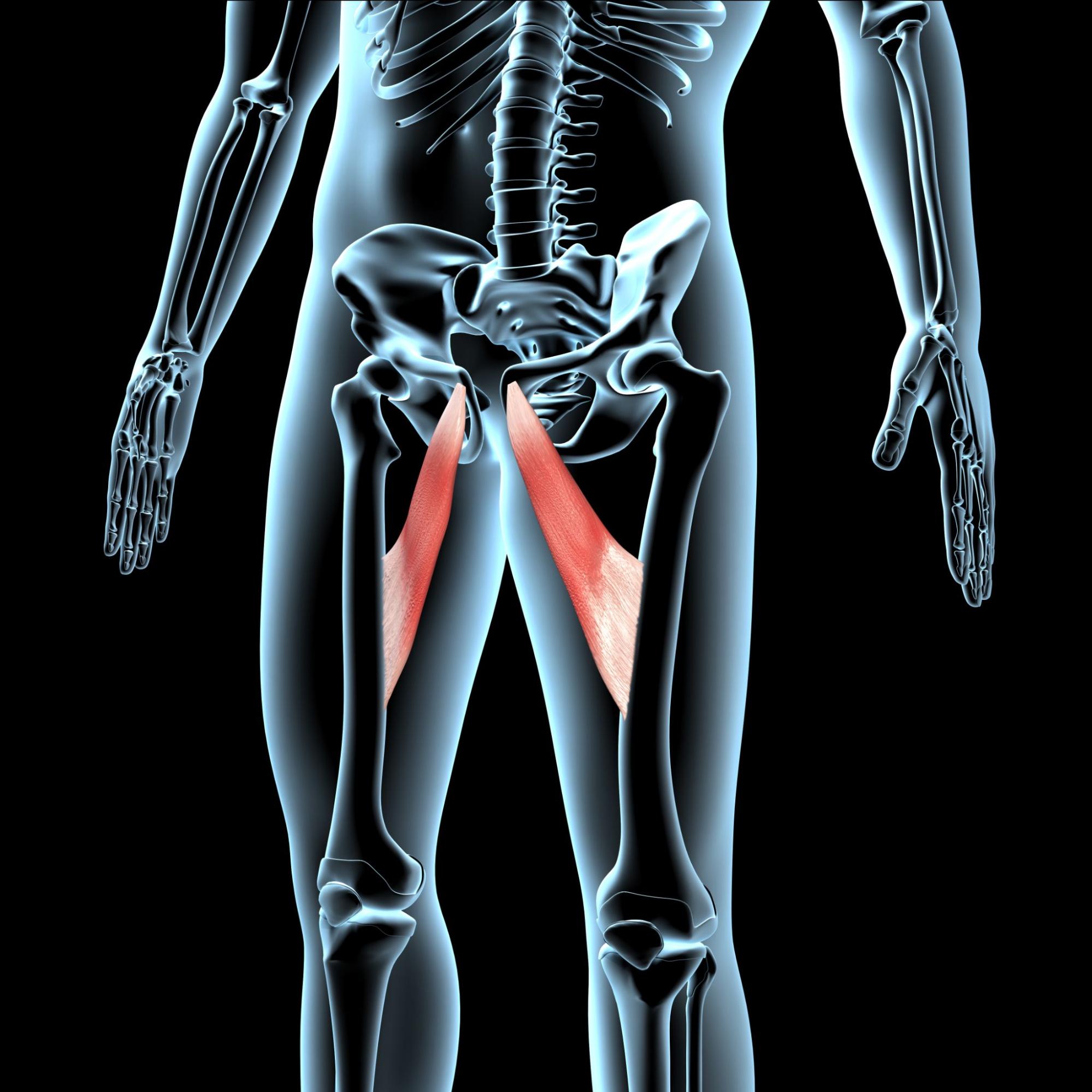
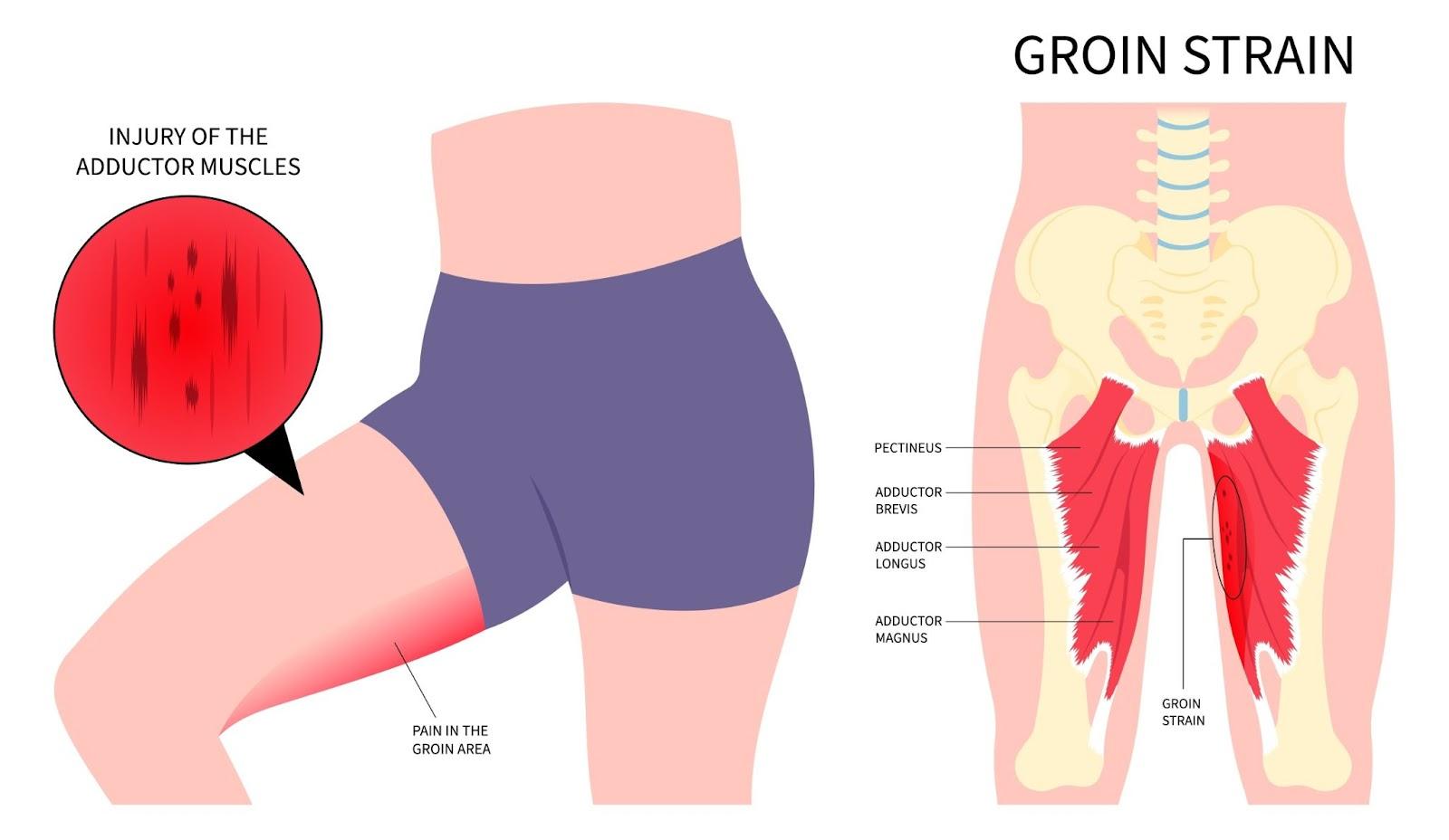
Adductor tendinopathy, also known as groin tendonitis, is a condition that affects the tendons of the adductor muscles, which are located along the inner thigh and play a crucial role in stabilising the pelvis and controlling leg movements. This condition is characterised by pain and dysfunction in the tendons that attach these muscles to the pubic bone, often resulting from repetitive stress, overuse, or biomechanical imbalances.
Unlike acute muscle strains, which occur suddenly due to trauma, adductor tendinopathy develops gradually over time due to excessive strain on the tendon. This strain leads to microtears, collagen degeneration, and an impaired ability of the tendon to withstand normal loading. If left untreated, the condition can progress to chronic pain and reduced function, particularly in activities that involve running, kicking, or rapid changes in direction.
Adductor tendinopathy is commonly observed in athletes involved in sports such as football, hockey, and running, where high levels of force are placed on the adductor tendons. However, it can also affect individuals with general lower limb weaknesses, poor movement mechanics, or those engaging in repetitive activities that strain the groin region.
Adductor tendinopathy is a chronic condition causing pain and dysfunction in the adductor tendons due to repetitive strain and tendon degeneration.
How adductor tendinopathy happens?
Adductor tendinopathy develops due to excessive mechanical loading on the adductor tendons, leading to structural and functional changes within the tendon tissue. The condition arises when the cumulative strain placed on the tendon surpasses its ability to repair and adapt, resulting in microscopic degeneration rather than an acute inflammatory response. Unlike tendonitis, which involves short-term inflammation, tendinopathy is a chronic process marked by collagen disruption, disorganisation of tendon fibres, and a loss of normal tendon elasticity.
During activities that involve high-force contractions, such as sudden accelerations, decelerations, and directional changes, the adductor muscles generate substantial force to stabilise the pelvis and control leg movement. If this force is applied repeatedly without adequate recovery, the tendon undergoes microtrauma at a rate that exceeds its natural repair capacity. Over time, this results in a maladaptive healing response, where healthy collagen is replaced with structurally inferior, disorganised tissue, which weakens the tendon and makes it more susceptible to pain and dysfunction.
In addition to tensile overload, compressive stress plays a crucial role in tendon degeneration, particularly at the insertion site where the adductor tendons attach to the pubic bone. When the tendon is repeatedly compressed against the bony interface—especially in hip flexion and abduction movements—this mechanical stress contributes to cell apoptosis, reduced collagen synthesis, and increased extracellular matrix breakdown. The combination of tensile strain and compressive load leads to changes in tendon composition, including neovascularisation and increased production of non-functional, disordered collagen fibres. This process impairs the tendon’s ability to transmit force efficiently, resulting in persistent pain and compromised function.
What are the common causes of adductor tendinopathy?
The common causes of adductor tendinopathy include:
- Repetitive strain and overuse
- Muscle imbalances and weakness
- Improper running or landing techniques
- Sudden increase in training load
- A history of groin strains or adductor injuries
- Tendon wear-and-tear
- Tight hip flexors or hamstrings
Adductor tendinopathy is caused by repetitive strain and excessive mechanical loading on the adductor tendons, leading to degeneration and impaired tendon healing.
What are the symptoms of adductor tendinopathy?
Adductor tendinopathy presents with a range of symptoms that develop gradually and worsen with continued activity. The key symptoms include:
- Groin pain – a dull, aching pain in the inner thigh or near the pubic bone, which may intensify with movement.
- Tenderness at the tendon insertion – sensitivity to touch along the pubic bone where the adductor tendons attach.
- Stiffness and discomfort – particularly noticeable in the morning or after prolonged periods of inactivity.
- Pain during movement – discomfort when bringing the legs together, squatting, running, or kicking.
- Weakness in the inner thigh – a sense of reduced strength or instability when engaging the adductor muscles.
- Pain with prolonged sitting – increased discomfort when seated for extended periods, especially with legs spread apart.
- Gradual onset and worsening symptoms – unlike acute muscle injuries, the pain tends to develop slowly and persist over time.
Symptoms may vary in intensity depending on the severity of the condition, with chronic cases leading to persistent pain that affects daily activities and sports performance.

Adductor tendinopathy can cause persistent groin pain, especially during activities involving hip movement, such as running, kicking, or changing direction.
Who is at risk of adductor tendinopathy in Singapore?
Adductor tendinopathy can affect individuals across various activity levels, but certain groups are more prone to developing the condition due to repetitive strain on the adductor tendons. In Singapore, the key risk factors include:
- Athletes in high-impact sports – footballers, runners, hockey players, and martial artists who frequently engage in rapid changes of direction, sprinting, or kicking.
- Recreational fitness enthusiasts – individuals participating in activities like CrossFit, HIIT workouts, and weightlifting, where explosive lower-body movements place excessive load on the adductor tendons.
- Dancers and gymnasts – those involved in ballet, contemporary dance, or gymnastics, which demand extreme hip mobility and sustained adductor activation.
- Office workers with prolonged sitting – sedentary individuals who remain seated for long hours, leading to muscular imbalances and weakened adductor tendons.
- Older adults with reduced tendon elasticity – ageing contributes to tendon degeneration, which makes older adults more vulnerable to tendinopathy (link to service page).
- Individuals with previous groin injuries – a history of adductor strains or groin pain increases the likelihood of developing chronic tendon issues.
- People with poor biomechanics – those with muscle imbalances, hip instability, or improper running and movement mechanics that place excessive strain on the adductor tendons.
How is adductor tendinopathy diagnosed?
At Cove Orthopaedics, we take a thorough and personalised approach to diagnosing adductor tendinopathy, which helps us ensure an accurate assessment and guide effective treatment. Our diagnostic process includes:
- Comprehensive clinical assessment – we begin with a detailed discussion of your symptoms, medical history, and activity levels to understand how the condition is affecting your daily life.
- Physical examination – our specialists assess for tenderness along the adductor tendon, pain with resisted hip adduction, and any movement restrictions that may indicate tendon dysfunction.
- Functional movement testing – we evaluate how your muscles and tendons respond during dynamic movements, such as squatting, lunging, and lateral movements, to identify patterns of strain and weakness.
- Ultrasound imaging – a high-resolution ultrasound scan helps us visualise tendon structure, detect degenerative changes, and assess the severity of the condition in real time.
- MRI scans (if needed) – in more complex cases, an MRI may be recommended to provide a detailed view of the tendons, surrounding muscles, and pubic bone to rule out other potential causes of groin pain.
By combining clinical assessment with specialised imaging techniques, we ensure a precise diagnosis and develop a treatment plan that targets the root cause of your symptoms and supports long-term recovery.
What are the treatment options for adductor tendinopathy?
We take a structured and comprehensive approach to treating adductor tendinopathy, focusing on reducing pain, restoring tendon health, and preventing recurrence. Depending on the severity of your condition, we utilise a range of treatment options, including:
- Activity modification – we guide you on adjusting your physical activity to reduce excessive strain on the tendon while maintaining overall mobility and fitness.
- Personalised physiotherapy programmes – targeted rehabilitation exercises help strengthen the adductor muscles, improve flexibility, and enhance movement mechanics to support tendon healing.
- Eccentric and isometric strengthening – we incorporate progressive loading exercises that promote tendon adaptation and restore its ability to tolerate stress.
- Manual therapy and soft tissue release – hands-on techniques, including deep tissue massage and myofascial release, can help alleviate muscle tightness and improve circulation in the affected area.
- Shockwave therapy – this non-invasive treatment stimulates tissue regeneration and promotes healing in chronic tendon conditions by increasing blood flow and breaking down dysfunctional collagen fibres.
- Ultrasound-guided injections – in cases of persistent pain, corticosteroid or platelet-rich plasma (PRP) injections may be used to provide relief and support tendon repair.
- Biomechanical assessment and correction – we analyse movement patterns and provide guidance on footwear, posture, and muscle imbalances to reduce strain on the adductor tendons.
- Gradual return-to-sport programmes – for athletes and active individuals, we develop structured rehabilitation plans to ensure a safe and effective return to training and competition.
Our goal is not only to relieve symptoms but also to address the underlying causes, so that we can help you regain strength and mobility while minimising the risk of future injury.
If you’re experiencing persistent groin pain or struggling with movement due to adductor tendinopathy, schedule a consultation with Cove Orthopaedics for a personalised assessment and personalised treatment plan that can help you get back to pain-free activity.
Frequently Asked Questions (FAQs)
How long does it take to recover from adductor tendinopathy?
Recovery time varies depending on the severity of the condition and adherence to treatment. With appropriate management, many individuals experience improvement within 4 to 12 weeks, while chronic cases may require up to six months for full recovery.
Can I continue exercising with adductor tendinopathy?
It’s important to modify activities to avoid aggravating the condition. Low-impact exercises that do not exacerbate groin pain, such as swimming or cycling, are generally recommended during recovery. Consult a physiotherapist who can tailor an exercise programme to your needs.
What are the potential complications if adductor tendinopathy is left untreated?
Without proper treatment, adductor tendinopathy can lead to chronic groin pain, reduced mobility, and an increased risk of tendon rupture, which may necessitate surgical intervention. Early diagnosis and management are crucial to prevent these complications.
Are there any preventive measures for adductor tendinopathy?
Yes, preventive strategies include incorporating proper warm-up and cool-down routines, gradually increasing the intensity and duration of workouts, and maintaining balanced muscle strength and flexibility through regular stretching and strengthening exercises targeting the hip and groin muscles.
When should I seek medical attention for groin pain?
If you experience persistent groin pain or discomfort, especially during physical activities, it’s advisable to consult a healthcare professional. Early diagnosis and treatment are essential for effective recovery and to prevent further complications.











