Hip Fracture

A hip fracture is the term used to describe fractures of the proximal femur, which is the upper part of the thigh bone that connects to the pelvis. Fractures can be anywhere from the femoral neck to the femoral shaft [1]. Hip fractures can cause significant morbidity and can be disabling. Understanding hip fractures, how they happen, risk factors, and treatment methods can help us identify an injury and seek the necessary treatment.
Anatomy of the hip
The hip is the ball and socket joint between the femur and the pelvis or hip bone. The primary function of the hip is to bear weight and to move your leg. Both the ‘socket’ of the pelvis (called the acetabulum) and ‘ball’ of the femur (called the femoral head) are covered in articular cartilage that allows movement [1]. Hip fractures occur in the femoral structures and are usually classified by the relationship to the hip capsule [2].
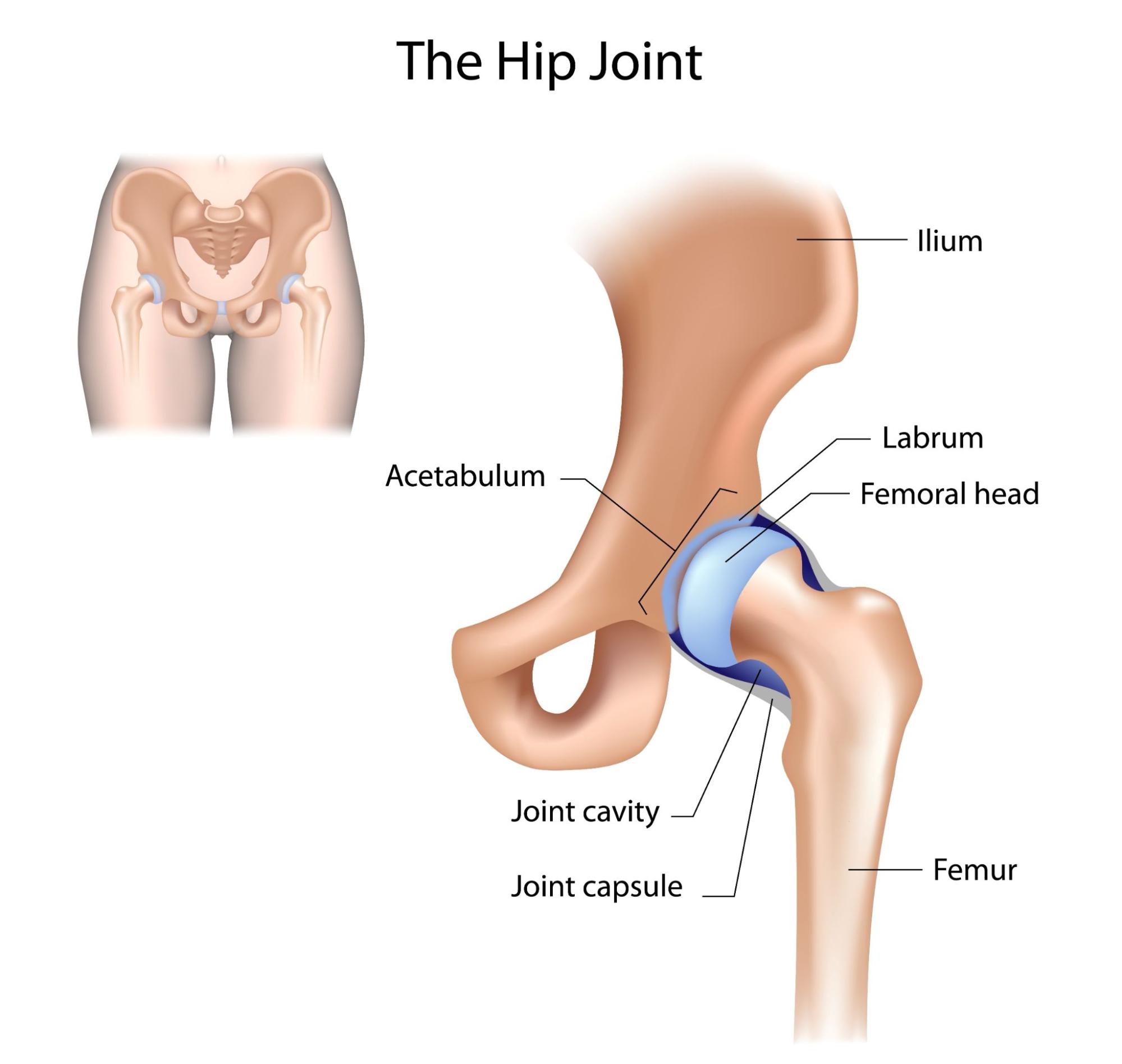
The hip consists of the pelvis and the proximal femur.
What are the types of hip fractures?
Hip fractures occur in relation to the position of the hip capsule. The types of fractures are:
Intracapsular –
Intracapsular hip fractures are fractures within the hip capsule, these typically consist of fractures that affect the femoral head and neck such as:
- Head fracture – Fractures of the femoral head.
- Subcapital fracture – Fractures that occur at the junction of the femoral head and femoral neck [2].
- Transcervical fracture – Fractures in the middle of the femoral neck [2].
- Basicervical fracture – Fractures at the base of the femoral neck, closer to the greater trochanter.
Extracapsular –
Extracapsular fractures happen outside of the hip capsule, these can include:
- Intertrochanteric fractures – Fractures between the femoral neck or greater trochanter and the lesser trochanter [1, 2].
- Subtrochanteric fractures – Fractures of the femoral shaft, usually within 5 cm of the lesser trochanter [1].
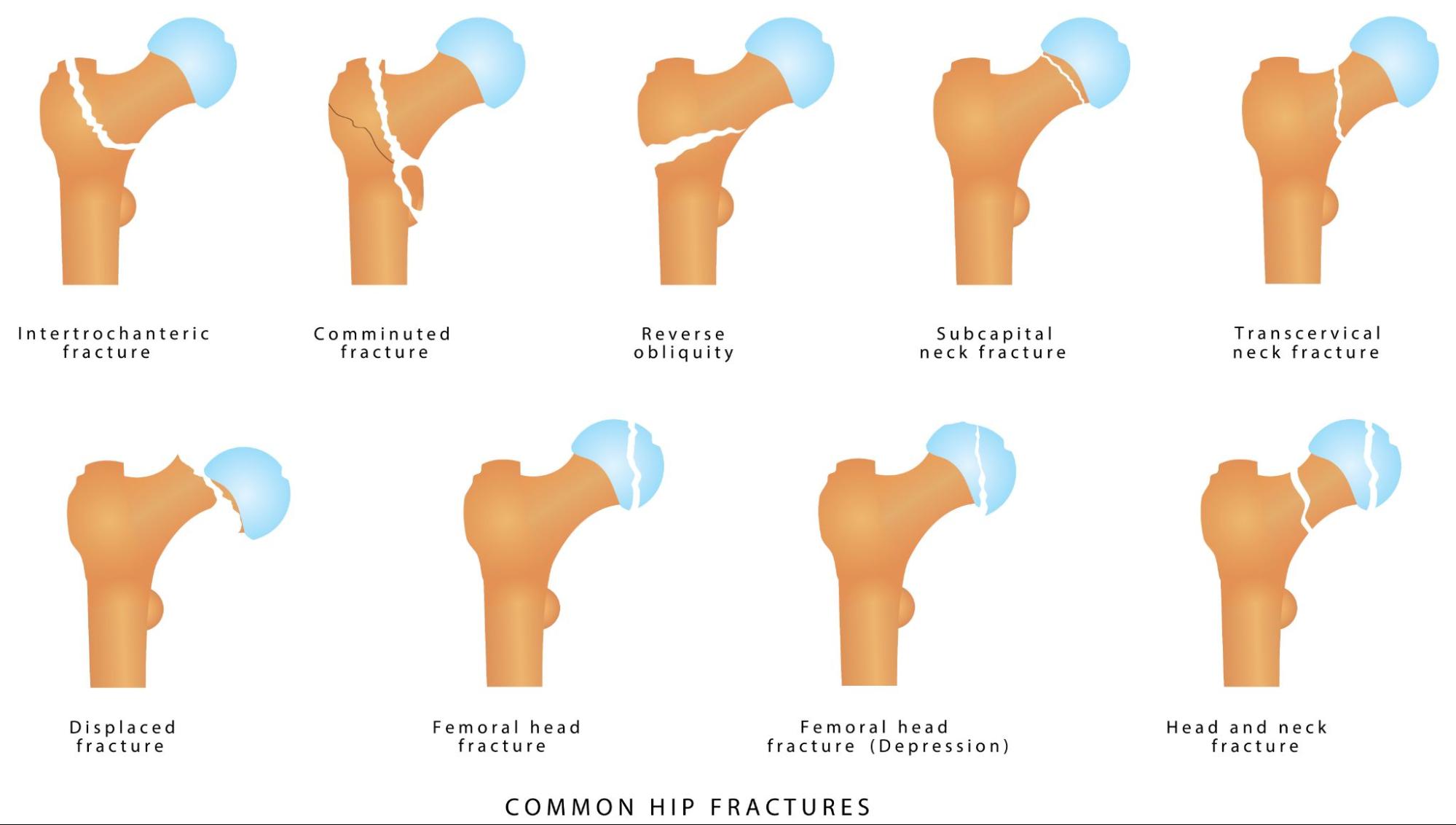
Hip fractures can be intracapsular or extracapsular fractures.
When an injury happens, we may not be able to tell which part of the hip is injured. However, knowing the type of injury is important for doctors and surgeons to determine the type of treatment, risks associated, and expected recovery outcome.
What are the symptoms of a Hip Fracture?
Symptoms of a hip fracture usually happen immediately or soon after an injury, like a fall or an accident. However, some fractures also happen with no history of injuries, these cases of hip fractures can include insufficiency fractures where it is caused by metabolic disorders or other conditions [1], or stress fractures where it is caused by wear and tear of the bone from repeated action. Common signs of a hip fractures include:
- Hip pain or groin pain
- Inability to stand or get up after a fall
- Inability to bear weight on the injured hip
- Injured leg may be shorter, abducted, or externally rotated
- Bruising or swelling of the hip region
What causes Hip Fractures?
Hip fractures can be caused by physical impact such as:
- Falls
- Car or motor accidents
- Sport injuries
However, in some cases hip fractures can be caused by the weakening of the bones from loss of bone density or wear and tear, leading to fractures from normal activities such as putting weight on the leg or twisting the hip.
What are the risk factors for Hip Fractures?
Hip fractures can happen to anyone, however several factors can increase the risk of getting fractures. These include:
- Age – Elderly people above the age of 65 are more likely to suffer from hip injuries compared to younger people [3]. This is due to the loss of bone density as we age.
- Sex – Women are more likely to get hip fractures compared to men. This is especially significant in elderly women as they lose bone density faster post-menopause [4].
- Medical conditions – Conditions that decrease bone density such as osteoporosis, or impair calcium and mineral absorption such as chronic kidney disease and intestinal diseases, can lead to weakened bones which eventually increases the risk of getting hip injuries from falls or accidents. Other medical conditions can also increase risks of injuries from falls due to poor coordination or balance, such as Parkinson’s disease, epilepsy, or gait abnormalities.
- Sports – Athletes who play contact sports are also more at higher risks of hip fractures mainly due to the increased risk of injuries.
- Medications – Chronic use of certain medications can increase the risk of fractures. This can be caused by the side effects of the medications. Such as:
- Levothyroxine – Loss of bone density
- Glucocorticoids – Loss of bone density, which leads to osteoporosis [5]
- Loop diuretics – Reduced calcium absorption in kidneys [3]
- Diet – A diet high in salt, caffeine, and alcohol can lead to loss of bone density due to the loss of calcium from the diet.
- Lack of physical activity – Lack of exercise can lead to weaker bones and muscles over time. Hence increasing the risk of fractures from minor injuries.
How are Hip Fractures diagnosed?
Hip fractures are associated with increased mortality, 17% to 30% of patients with a hip fracture die within the first year [1, 2, 3]. Hence, early diagnosis and treatment of hip fractures can potentially improve a patient’s quality of life and life expectancy.
If you are experiencing the signs and symptoms of a hip fracture, a prompt visit to the orthopaedic clinic is important. Some fractures may not show obvious deformities, however hip fractures can largely impact ability to function or live independently, hence affecting quality of life.
In an orthopaedic clinic, doctors will perform several tests to diagnose a hip fracture:
- Physical test – During a physical examination, the doctor will observe for any abnormalities of the hip and leg. The doctor will also assess pain when rotation is applied to the leg. Sometimes the doctor may ask you to perform leg raises [3].
- X-ray imaging – X-ray imaging or radiography is almost always the first test to diagnose a hip fracture. Typically the radiograph is taken from the ‘front to back’, also called the anteroposterior view, this is also accompanied with an image from a different angle to assess the cause of the hip pain [6].
- Magnetic resonance imaging (MRI) – If a fracture is not detected from an X-ray, an MRI can be done to identify any stress fractures, muscle, or cartilage injuries [6].
- Computed tomography (CT) – CT scans are not typically used in the diagnosis of hip fractures, but can be done to examine injuries of the cartilage [6].
How are Hip Fractures treated?
Treatment of hip fractures will vary according to the type or location of injury, severity of injury, and patient condition. Common methods of hip fracture treatment are:
- Open reduction and internal fixation (ORIF) – Fixation treatments are commonly used in nondisplaced or minimally displaced femoral neck fractures. This method involves using specialised screws to fix the bones in place [2].
- Arthroplasty – Arthroplasty is a total hip replacement. Arthroplasty involves replacing the whole hip joint, which are the acetabulum and the femoral head [3]. This method can be used to treat displaced femoral neck fractures or femoral head fractures. The surgical procedure for a total arthroplasty is more expensive and complicated, but it is associated with better functional outcomes and is therefore recommended for younger and more active patients to regain leg and hip function [2].
- Hemiarthroplasty – Hemiarthroplasty is also called partial hip replacement. Hemiarthroplasty involves replacing only the femoral head. This method is more cost effective, with less operative time and less blood loss. However, follow-up studies have found that hemiarthroplasty surgeries have higher revision rates compared to arthroplasty surgeries [2]. Ultimately, the choice of the surgery will depend on the patient and the injury.
- Extramedullary fixation – Extramedullary fixation involves applying plates and screws on the lateral side of the femur [7]. This method is typically used for extracapsular fractures.
- Intramedullary fixation – Intramedullary fixation is a surgical method that involves inserting a rod into the femur. This type of surgery provides better stability to the bone, and is typically used in intertrochanteric fractures [2].
Post-operative care –
- Patients who underwent arthroplasty or hemiarthroplasty surgery may be required to come for follow-up X-rays to ensure proper positioning of the prostheses.
- Physical therapy or rehabilitation should be done as soon as advisable, as reduced mobility increases the risk of deep vein thrombosis and pulmonary embolism [1].
- Strategies to prevent further hip injuries should be enforced, such as installing hand railings, removing clutter from homes, and using non-slip mats.
Treatments for hip fractures are very personalised to the patient’s case, your doctor will perform the ideal treatment for your injury and advise you on what you can or cannot do while recovering from the surgery.
Complications of hip fractures
Hip fractures can negatively impact your life. Increased morbidity and mortality is associated with hip fractures. Risks of complications also increase when treatment is delayed. Some of these complications include:
- Inability to live independently
- Muscle wasting from reduced mobility
- Blood clots forming in the legs or lungs (deep vein thrombosis and pulmonary embolism)
- Bedsores from lying in bed too long
- Pneumonia
Hip injuries can happen to anyone, but morbidity and mortality is higher in high risk individuals. If you or a loved one is suffering from a suspected hip fracture, a visit to the orthopaedic clinic is crucial to diagnose and treat the fracture. Early treatment can improve recovery and can be potentially life-saving.
Reach out to us now to schedule an appointment if you are in need of a diagnosis for hip injuries.
What can I expect during a Hip Fracture recovery?
A hip fracture can be a serious injury and will take time to heal. Depending on the severity of the fracture, it may take anywhere between 3 months to a year.
- Recovery from surgery – Recovery from surgery typically takes about 6 weeks. During this time, you may not be able to walk on your own.
- Physical therapy – For the next several months (about 6 to 9 months), you may require physical therapy to regain your leg strength and function.
- Full recovery – Full recovery of your hip and legs may take anywhere between 9 months to a year. In some cases, patients may not be able to regain their full strength and mobility before the injury.
Summary
Hip fractures are a serious injury and can potentially be life threatening, immediate medical attention is crucial in case of traumatic injuries or accidents. Furthermore, delay in treatment can also increase the risk of serious complications and incomplete recovery.
Call emergency services immediately if you or a loved one experience signs of hip fractures. For other concerns about hip fractures, reach out to us to book an appointment with our doctor for a detailed analysis and personalised treatment plan.
Frequently Asked Questions
How can I prevent hip fractures?
Certain modifiable risk factors of hip fractures include diet, exercise, and use of medication. Maintaining a healthy diet with sufficient calcium and vitamin D, doing exercises regularly, and limiting the use of medications that lead to bone loss can help maintain healthy and strong bones even in old age. Other prevention steps can include measures to reduce falls and accidents especially in elderly people.
How long does it take to recover from a hip fracture surgery?
Healing time varies depending on the type of surgery, the type of injury, your age and general health condition. Recovery can take anywhere between several weeks to 3 months. It may also take anywhere between 6 months to a year for your leg to regain its full strength.
Can you move with a broken hip?
You may not be able to move or walk with a broken hip, moving someone with a broken hip may also increase the risk of further injuries. Contacting emergency services is important when helping someone with a broken hip.
References
- Li L, Bennett-Brown K, Morgan C, Dattani R. Hip fractures. Br J Hosp Med (Lond). 2020 Aug 2;81(8):1-10. doi: 10.12968/hmed.2020.0215. PMID: 32845763.
- Lu Y, Uppal HS. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr Orthop Surg Rehabil. 2019 Jul 3;10:2151459319859139. doi: 10.1177/2151459319859139. PMID: 31321116; PMCID: PMC6610445.
- LeBlanc KE, Muncie HL Jr, LeBlanc LL. Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician. 2014 Jun 15;89(12):945-51. PMID: 25162161.
- Banks E, Reeves GK, Beral V, Balkwill A, Liu B, Roddam A; Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis. PLoS Med. 2009 Nov;6(11):e1000181. doi: 10.1371/journal.pmed.1000181. Epub 2009 Nov 10. PMID: 19901981; PMCID: PMC2766835.
- Briot K, Roux C. Glucocorticoid-induced osteoporosis. RMD Open. 2015 Apr 8;1(1):e000014. doi: 10.1136/rmdopen-2014-000014. PMID: 26509049; PMCID: PMC4613168.
- Blankenbaker DG, De Smet AA. Hip injuries in athletes. Radiol Clin North Am. 2010 Nov;48(6):1155-78. doi: 10.1016/j.rcl.2010.07.003. PMID: 21094404.
- Parker MJ, Handoll HH, Chinoy MA. Extramedullary fixation implants for extracapsular hip fractures. Cochrane Database Syst Rev. 2001;(2):CD000339. doi: 10.1002/14651858.CD000339. Update in: Cochrane Database Syst Rev. 2002;(2):CD000339. doi: 10.1002/14651858.CD000339. PMID: 11405960.











