Ischial
Bursitis
- Home
- Conditions We Treat
- Hip
- Ishchial Bursitis
What is Ischial Bursitis?
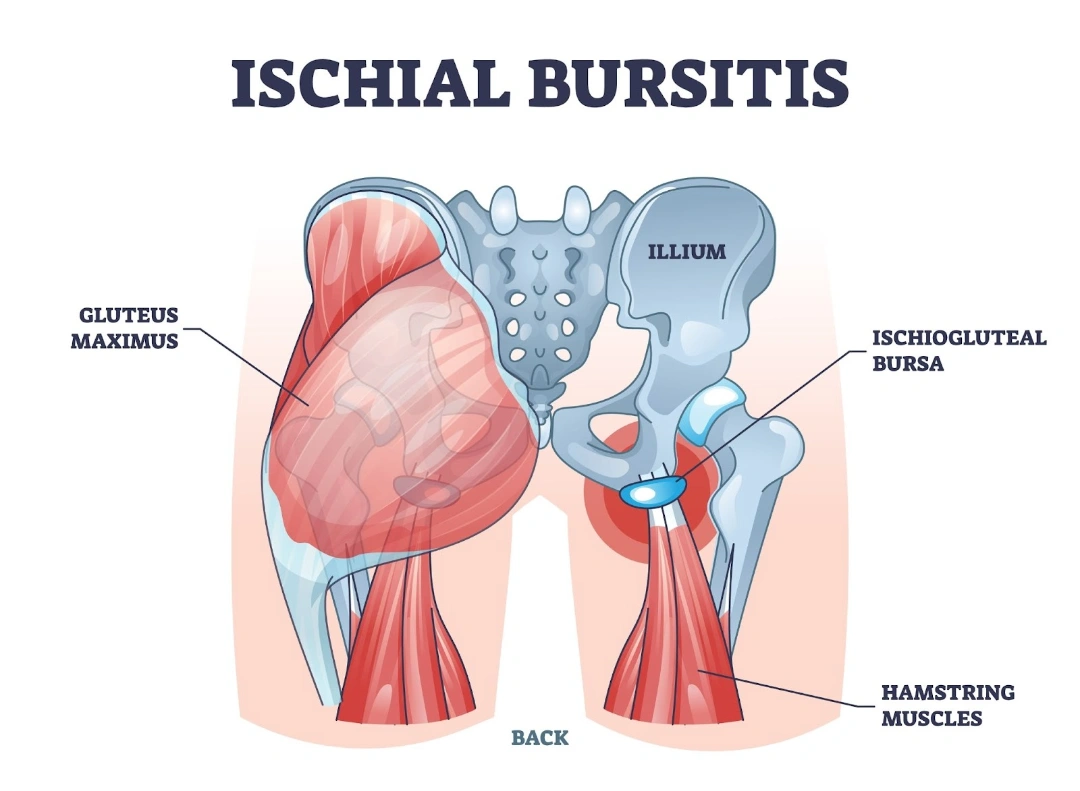
Ischial bursitis, also known as weaver’s bottom or sitz bone bursitis, is a condition that results from inflammation of the ischial bursa, a small fluid-filled sac located between the ischial tuberosity (the bony prominence at the base of the pelvis) and the surrounding soft tissues. The ischial bursa functions as a cushion, reducing friction between the bones and muscles when sitting or engaging in activities that involve repetitive hip movement.
When this bursa becomes inflamed, it can cause localised pain, tenderness, and discomfort, particularly when sitting on hard surfaces or engaging in prolonged periods of seated activity. The condition is commonly associated with occupations or activities that involve extended sitting, such as cycling, rowing, or driving, as well as certain sports that require repetitive hip extension, including running and gymnastics.
Although ischial bursitis can be managed with conservative treatments, persistent cases may require targeted interventions. Early diagnosis and appropriate management can help prevent worsening symptoms and improve overall function.

What causes Ischial Bursitis?
Ischial bursitis occurs when the ischial bursa—a small, fluid-filled sac that reduces friction between the ischial tuberosity (the bony prominence at the base of the pelvis) and surrounding tissues—becomes inflamed. This inflammation is primarily triggered by prolonged pressure, repetitive movements, or underlying medical conditions that contribute to excessive friction or irritation in the area. Common causes of ischial bursitis include the following:
- Prolonged sitting — spending long hours sitting, particularly on hard or unpadded surfaces, increases the risk of bursal irritation. Sustained pressure compresses the bursa, leading to inflammation over time.
- Repetitive hip movements — activities that involve frequent hip extension and flexion, such as cycling, rowing, running, and certain forms of weight training, can place excessive stress on the ischial bursa. The repetitive friction between the hamstring tendons and the bursa contributes to microtrauma and inflammation, which increases the likelihood of developing bursitis.
- Direct trauma or injury — a fall or a direct blow to the buttocks can result in acute inflammation of the ischial bursa. Sports injuries, accidents, or even prolonged pressure from hard seating after an injury may aggravate the bursa, leading to pain and discomfort.
- Muscle imbalances and tightness — tight or weak hamstrings and gluteal muscles can alter the biomechanics of the hip and pelvis, leading to increased friction over the ischial tuberosity. Athletes or individuals who fail to stretch properly before engaging in physical activity may experience excessive strain in this region, heightening the risk of bursitis.
- Poor posture and biomechanics — improper posture while sitting, walking, or engaging in physical activities can contribute to ischial bursitis. Slouching, sitting with uneven weight distribution, or using poorly designed seating arrangements can place continuous strain on the ischial bursa, leading to irritation and inflammation.
- Underlying medical conditions — certain systemic conditions can predispose individuals to ischial bursitis by promoting inflammation and joint-related issues. These include:
- Rheumatoid arthritis – an autoimmune disorder that causes chronic inflammation in the joints and surrounding bursae.
- Gout – a condition that results from excess uric acid in the blood, leading to crystal deposits in joints and bursae, causing painful inflammation.
- Osteoarthritis – Osteoarthritis involves the degeneration of cartilage in joints, which can lead to increased friction and irritation in the bursa.
- Post-surgical or structural changes — individuals who have undergone hip or lower back surgery may experience altered movement patterns that put extra stress on the ischial bursa. Similarly, anatomical abnormalities or limb-length discrepancies can contribute to an uneven gait, increasing the risk of bursal irritation.
What are the symptoms of Ischial Bursitis?

Ischial bursitis primarily causes discomfort in the lower buttock region, particularly when sitting or engaging in repetitive movements that put pressure on the ischial tuberosity. Symptoms can vary in severity, ranging from mild irritation to persistent pain that affects daily activities. Common symptoms of ischial bursitis include:
- Pain and tenderness in the buttock region — a deep, aching discomfort is typically felt over the ischial tuberosity, which may worsen with prolonged sitting.
- Discomfort when sitting on hard surfaces — symptoms often intensify when seated on firm chairs or benches for extended periods.
- Pain radiating down the posterior thigh — the discomfort may extend along the hamstring, which mimics sciatic nerve pain.
- Swelling or warmth over the ischial tuberosity — inflammation of the bursa can cause mild swelling, redness, or a sensation of warmth in the affected area.
- Stiffness or reduced mobility — tightness in the surrounding muscles may limit movement, particularly during activities like running, walking, or stretching the hamstrings.
- Increased pain with repetitive activities — movements that involve repeated hip flexion and extension, such as cycling or rowing, can exacerbate symptoms.
Who is at risk of Ischial Bursitis in Singapore?
Ischial bursitis can affect individuals across different age groups and lifestyles, but certain factors increase the likelihood of developing this condition. In Singapore, where sedentary work environments and physically demanding activities are both common, several groups are particularly at risk. People at higher risk of Ischial Bursitis include:
- Office workers and professionals — long hours of desk work and prolonged sitting in office chairs can increase pressure on the ischial bursa, leading to inflammation over time.
- Cyclists and endurance athletes — regular participation in cycling, rowing, long-distance running, or other sports that involve repetitive hip movement can put excessive strain on the ischial tuberosity.
- Elderly individuals — age-related muscle weakness and joint degeneration, including osteoarthritis, can increase the risk of bursitis.
- Drivers and delivery personnel — taxi, private-hire, and delivery drivers who spend extended periods sitting may experience chronic pressure on the ischial region.
- Gym-goers and weightlifters — certain exercises, such as squats and deadlifts, may contribute to bursitis if performed with poor form or without proper recovery.
- Patients with inflammatory conditions — individuals with rheumatoid arthritis, gout, or other inflammatory joint disorders are more prone to bursitis due to systemic inflammation.
- People with poor posture or muscle imbalances — weak or tight hamstrings and gluteal muscles, combined with poor sitting posture, can increase friction over the ischial bursa, making inflammation more likely.
How is Ischial Bursitis diagnosed?
Since the symptoms can overlap with other conditions, such as hamstring tendinopathy or sciatica, an accurate diagnosis is essential for effective treatment. Our approach to diagnosing Ischial Bursitis includes the following:
- Comprehensive medical history and symptom assessment — we start by understanding your symptoms, lifestyle, and any activities that may be contributing to your discomfort. Details such as the duration of pain, aggravating factors, and previous injuries help us determine whether ischial bursitis is the likely cause.
- Physical examination — our specialists perform a targeted examination to assess tenderness over the ischial tuberosity, evaluate mobility, and check for pain during movements like sitting, walking, or stretching the hamstrings. Specialised clinical tests help differentiate ischial bursitis from other conditions affecting the lower back and pelvis.
- Ultrasound imaging — ultrasound scans are used to detect inflammation in the ischial bursa and assess any associated soft tissue abnormalities. Ultrasound is a quick, non-invasive method that provides real-time imaging to aid in diagnosis.
- X-rays — while X-rays do not show soft tissue inflammation, they can help rule out underlying issues such as bony spurs, fractures, or arthritis that may be contributing to your symptoms.
- MRI scans — in cases where a more detailed assessment is needed, an MRI can provide high-resolution images of the ischial bursa, surrounding tendons, and muscles to confirm inflammation and detect any structural abnormalities.
What are the treatment options for Ischial Bursitis in Singapore?
Treatment is determined based on the severity of symptoms and the patient’s lifestyle, which helps us ensure effective relief and long-term recovery. In most cases, conservative treatments provide significant improvement, but for persistent or severe cases, complex interventions may be necessary.
- Activity modification and ergonomic adjustments — we guide our patients on making lifestyle changes to reduce pressure on the ischial bursa. This includes using cushioned seating, avoiding prolonged sitting on hard surfaces, and incorporating regular movement breaks into daily routines.
- Physiotherapy and stretching exercises — our physiotherapists design customised rehabilitation programmes to strengthen the surrounding muscles, improve flexibility, and reduce strain on the ischial bursa. Stretching exercises targeting the hamstrings and gluteal muscles help alleviate tension and promote healing.
- Medications for pain and inflammation — we may recommend nonsteroidal anti-inflammatory drugs (NSAIDs) to help reduce pain and swelling, particularly for patients experiencing acute discomfort. These medications are typically used in conjunction with other treatment strategies.
- Ultrasound-guided corticosteroid injections — for patients with persistent pain, we offer targeted corticosteroid injections to reduce inflammation and provide lasting relief. Ultrasound guidance ensures precision and effectiveness, which helps minimise discomfort and enhance results.
- Shockwave therapy — in some cases, we incorporate extracorporeal shockwave therapy (ESWT) to stimulate healing, reduce inflammation, and break down scar tissue in the affected area. This non-invasive treatment is particularly beneficial for chronic cases of ischial bursitis.
- Platelet-rich plasma (PRP) therapy — for patients seeking regenerative treatment options, PRP therapy may be considered to promote tissue healing and reduce inflammation naturally. This involves using a concentrated solution of the patient’s own platelets to accelerate recovery.
- Surgical intervention (rare cases) — while surgery is rarely required, in severe or chronic cases that do not respond to conservative treatments, surgical removal of the inflamed bursa (bursectomy) may be considered.
Summary
Ischial bursitis often presents as a deep ache in the lower buttock, particularly noticeable when sitting for extended periods or stretching the hamstrings. It is typically caused by inflammation of the bursa over the ischial tuberosity, often due to prolonged pressure, repetitive strain, or direct trauma.
Although symptoms may begin mildly, persistent discomfort can interfere with daily activities over time. If the pain continues or worsens, do seek an orthopaedic specialist for a medical consultation. Schedule an appointment with us today for a detailed assessment and personalised treatment plan.
Conditions We Treat





Frequently asked questions
Can ischial bursitis cause sciatica-like symptoms?
Yes, ischial bursitis can cause pain that radiates down the back of the thigh, similar to sciatica. However, sciatica is due to nerve compression, while ischial bursitis stems from inflammation of the bursa near the ischial tuberosity.
How long does it take to recover from ischial bursitis?
Recovery time varies depending on the severity and treatment approach. With appropriate rest and conservative management, symptoms often improve within a few weeks.
Can ischial bursitis become a chronic condition?
If not properly managed, ischial bursitis can become chronic, leading to persistent discomfort and functional limitations. Early intervention and adherence to treatment recommendations are crucial for preventing recurrence.
Are there any complications associated with untreated ischial bursitis?
Untreated ischial bursitis can lead to chronic pain, reduced mobility, and in rare cases, infection of the bursa.
What lifestyle modifications can help prevent ischial bursitis?
To prevent ischial bursitis, avoid prolonged sitting on hard surfaces, incorporate regular breaks during sedentary activities, and engage in exercises that strengthen and stretch the hip and gluteal muscles.



