What is Hip Osteoarthritis?
Hip osteoarthritis is a chronic, degenerative joint condition that affects the hip, one of the body’s largest and most active joints. It occurs when the protective cartilage cushioning the ends of the bones in the hip joint gradually wears away. This cartilage is essential for smooth, pain-free movement, and its breakdown results in increased friction between the bones, leading to inflammation, pain, and stiffness.
The hip joint is a ball-and-socket structure, where the femoral head (the ball) fits into the acetabulum (the socket) of the pelvis. In a healthy joint, cartilage ensures smooth movement and absorbs shock during activities like walking and running. However, as the cartilage erodes, bones rub against each other, resulting in bone spurs, narrowing of the joint space, and progressive symptoms that affect daily life.
Hip osteoarthritis progresses through several stages and can stem from different underlying causes.
What are the stages of Hip Osteoarthritis?
|
Stages of Hip Osteoarthritis |
Description |
|
Stage 1 |
Minor cartilage wear and small bone spurs, often without noticeable pain or symptoms. |
|
Stage 2 (Mild) |
Cartilage breakdown begins, with visible bone spurs on X-rays. Pain, stiffness, and discomfort start to appear. |
|
Stage 3 (Moderate) |
Significant cartilage erosion and narrowing of the joint space. Pain and swelling occur during daily activities like walking or kneeling. |
|
Stage 4 (Severe) |
Advanced cartilage loss leads to chronic pain, stiffness, and joint inflammation, even at rest. |
Types of Hip Arthritis
|
Type |
Description |
|
Rheumatoid Arthritis |
An autoimmune condition where the immune system attacks healthy tissue, causing inflammation of the synovial membrane and gradual cartilage breakdown. Symptoms may not affect the hip initially but progress over time. |
|
Psoriatic Arthritis |
Linked to psoriasis, this autoimmune disorder causes inflammation in the hip joint, leading to damage if untreated. It may occur before or after skin symptoms. |
|
Post-Traumatic Arthritis |
Results from hip injuries like fractures or trauma. Even after the injury heals, cartilage damage or joint misalignment can lead to arthritis later in life. |
|
Avascular Necrosis |
Occurs when the femoral head loses its blood supply, causing bone collapse and eventual severe arthritis due to joint deformity. |
Hip osteoarthritis is a progressive disease, meaning it worsens over time, and early diagnosis and intervention are crucial to managing its symptoms and preventing further joint damage.
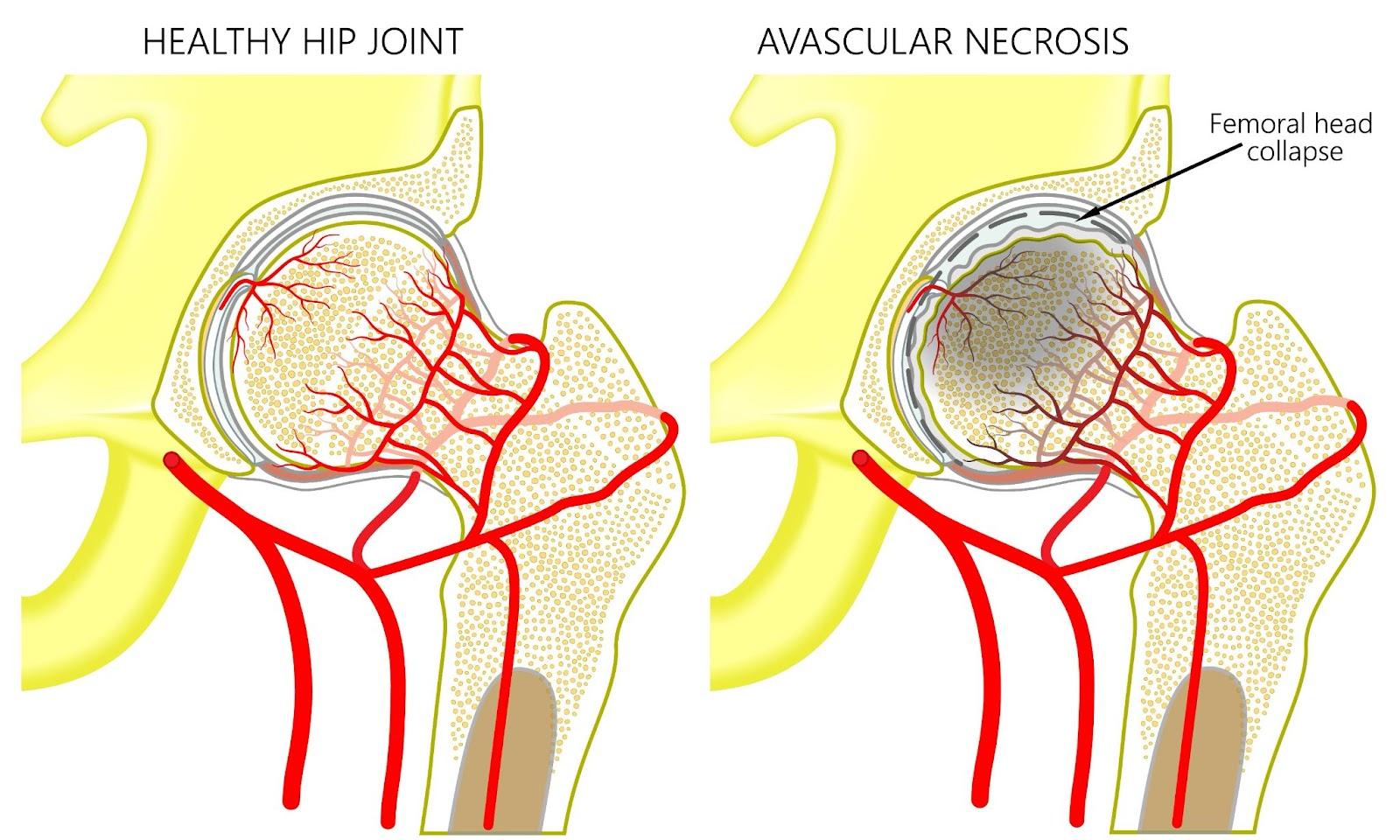
In a healthy hip joint, cartilage ensures smooth movement and cushioning, while in avascular necrosis, the bone loses blood supply, leading to collapse and joint damage.
What causes Hip Osteoarthritis?
Hip osteoarthritis develops due to the gradual breakdown of articular cartilage, a smooth, resilient tissue that covers the ends of the bones within the hip joint. This cartilage serves as a cushion, reducing friction and absorbing impact during movement. The condition begins when the cartilage matrix, composed of collagen and proteoglycans, deteriorates due to an imbalance between its synthesis and degradation.
As the cartilage wears away, the bones within the joint lose their protective buffer, leading to increased mechanical stress and friction. This friction triggers an inflammatory response, releasing enzymes and pro-inflammatory mediators, such as cytokines, which further accelerate cartilage degradation. Over time, the underlying bone responds by forming osteophytes (bone spurs) and thickening, while the joint space narrows. These changes disrupt the smooth mechanics of the hip joint, causing pain, stiffness, and reduced mobility, ultimately affecting its function.
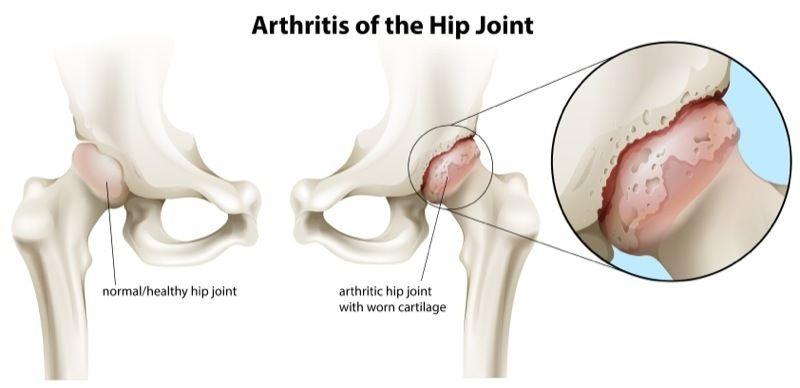
Hip osteoarthritis is caused by the gradual breakdown of cartilage in the hip joint, leading to increased friction and joint damage.
What are the symptoms of Hip Osteoarthritis?
Hip osteoarthritis often develops gradually, and its symptoms can range from mild discomfort to severe pain that significantly affects daily life. Recognising these symptoms early can help in managing the condition effectively. Common signs include:
- Pain in the hip joint — often felt in the groin, thigh, or buttocks, especially during or after movement.
- Stiffness — difficulty moving the hip joint, particularly after periods of inactivity or in the morning.
- Swelling and inflammation — visible or palpable swelling around the hip joint.
- Grinding or clicking sensations — a feeling or sound of the bones rubbing against each other during movement.
- Limited range of motion — difficulty performing tasks like bending, walking, or climbing stairs.
- Radiating pain — discomfort that extends to the knee or lower back.
- Weakness in the hip area — a feeling of instability or reduced strength in the joint.
These symptoms may worsen with physical activity or as the condition progresses, which may impact your ability to perform everyday tasks. Early diagnosis and treatment can help mitigate these effects and preserve joint health.

Hip osteoarthritis causes persistent hip joint pain, often felt in the groin, thigh, or buttocks, which worsens with activity and impacts daily life.
Who is at risk of hip osteoarthritis in Singapore?
Hip osteoarthritis can develop in anyone, but certain factors can significantly increase the risk. By understanding these risks, individuals can take steps to manage or reduce their chances of developing the condition. Those at higher risk include:
- Older adults — natural ageing leads to cartilage wear, which makes osteoarthritis more common in older individuals.
- Family history — a genetic predisposition may increase the likelihood of joint degeneration.
- Previous joint injuries — injuries such as hip fractures or dislocations can accelerate cartilage breakdown.
- Obesity or excess weight — carrying extra weight puts additional stress on the hip joints, hastening wear and tear.
- Autoimmune triggers — conditions like rheumatoid arthritis or psoriatic arthritis, potentially triggered by infections or immune responses, can contribute to joint damage.
- Other health conditions — diabetes, high cholesterol, vitamin D deficiency, and hemochromatosis (excess iron in the blood) are linked to an increased risk of osteoarthritis.
- Hormonal changes in women — post-menopausal women may have a higher risk due to hormonal shifts affecting joint health.
- Hip abnormalities — congenital or developmental disorders, such as hip dysplasia, can predispose individuals to earlier cartilage degeneration.
- Repetitive stress from activities or occupations — physically demanding jobs or sports that involve repetitive hip movements or heavy lifting can strain the hip over time.
By addressing modifiable risk factors, such as weight management and monitoring other health conditions, individuals can reduce their risk of developing hip osteoarthritis and maintain better joint health.
How is hip osteoarthritis diagnosed?
At Cove Orthopaedics, we are committed to providing accurate diagnoses and personalised care for hip osteoarthritis. By utilising a comprehensive approach, we ensure that every patient receives the most effective treatment tailored to their needs. Our diagnostic process typically involves the following:
- Detailed medical history — we begin by discussing your symptoms, lifestyle, and any prior injuries to understand your condition better.
- Physical examination — our specialists assess your hip’s range of motion, joint stability, and areas of tenderness to pinpoint the problem.
- Imaging tests — X-rays are commonly used to detect joint space narrowing, bone spurs, and other changes indicative of osteoarthritis. In some cases, we may recommend imaging tests like MRI to evaluate soft tissue and cartilage damage.
- Lab tests — to rule out other conditions, such as rheumatoid arthritis or infections, we may conduct blood tests or analyse joint fluid.
- Functional assessments — we evaluate how your hip osteoarthritis impacts your daily activities, which helps us create a treatment plan that restores your mobility and quality of life.
At Cove Orthopaedics, our expertise and patient-centric approach ensure that you receive a thorough diagnosis and a clear understanding of your condition and treatment options.
What are the treatment options for hip osteoarthritis in Singapore?
At Cove Orthopaedics, we offer a range of effective treatment options according to your health condition and needs, aiming to reduce pain, improve mobility, and enhance your quality of life. Depending on the severity of your condition and your personal circumstances, our treatment options include:
- Lifestyle modifications — our healthcare experts guide you in making adjustments to reduce joint strain, such as weight management and activity modification.
- Physical therapy — our specialists design personalised exercise programs to strengthen the muscles surrounding your hip and improve flexibility.
- Medications — we may prescribe pain relievers, anti-inflammatory medications, or topical treatments to alleviate discomfort.
- Injections — in some cases, we opt for corticosteroid injections that can reduce inflammation, and hyaluronic acid injections that help improve joint lubrication and mobility.
- Assistive devices — walking aids, such as canes or walkers, can help reduce stress on the hip joint.
- Minimally invasive procedures — for moderate cases, we may recommend arthroscopy to repair or clean the joint.
- Surgical options — in severe cases where other treatments are no longer effective, we perform total hip replacement surgery to restore function and relieve chronic pain.
If you are struggling with hip pain or stiffness due to osteoarthritis, don’t let it hold you back. Schedule a consultation with Cove Orthopaedics today to explore personalised treatment options and take the first step toward reclaiming your mobility and comfort.
Frequently Asked Questions (FAQs)
Can hip osteoarthritis be prevented?
While it’s not always possible to prevent hip osteoarthritis, certain lifestyle choices can reduce your risk. Maintaining a healthy weight, engaging in regular low-impact exercise, and avoiding joint injuries can help preserve hip joint health.
Is hip osteoarthritis hereditary?
Genetics can play a role in the development of hip osteoarthritis. If you have a family history of the condition, you may be at a higher risk. However, environmental factors and lifestyle choices also significantly influence its onset.
What complications can arise from untreated hip osteoarthritis?
If left untreated, hip osteoarthritis can lead to chronic pain, decreased mobility, and reduced quality of life. In severe cases, it may result in disability or necessitate joint replacement surgery.
How does hip osteoarthritis affect daily activities?
Hip osteoarthritis can make everyday tasks like walking, climbing stairs, or standing for extended periods challenging due to pain and stiffness. This can impact your ability to work, exercise, and perform household chores.
Can hip osteoarthritis be treated without surgery?
Yes, hip osteoarthritis can often be managed without surgery, especially in its early to moderate stages. Non-surgical treatments include physical therapy, medications, lifestyle modifications, assistive devices, and injections like corticosteroids or hyaluronic acid. These approaches aim to alleviate pain, improve mobility, and slow disease progression.











