Pelvic
Fractures
- Home
- Conditions We Treat
- Hip
- Pelvic Fractures
Introduction
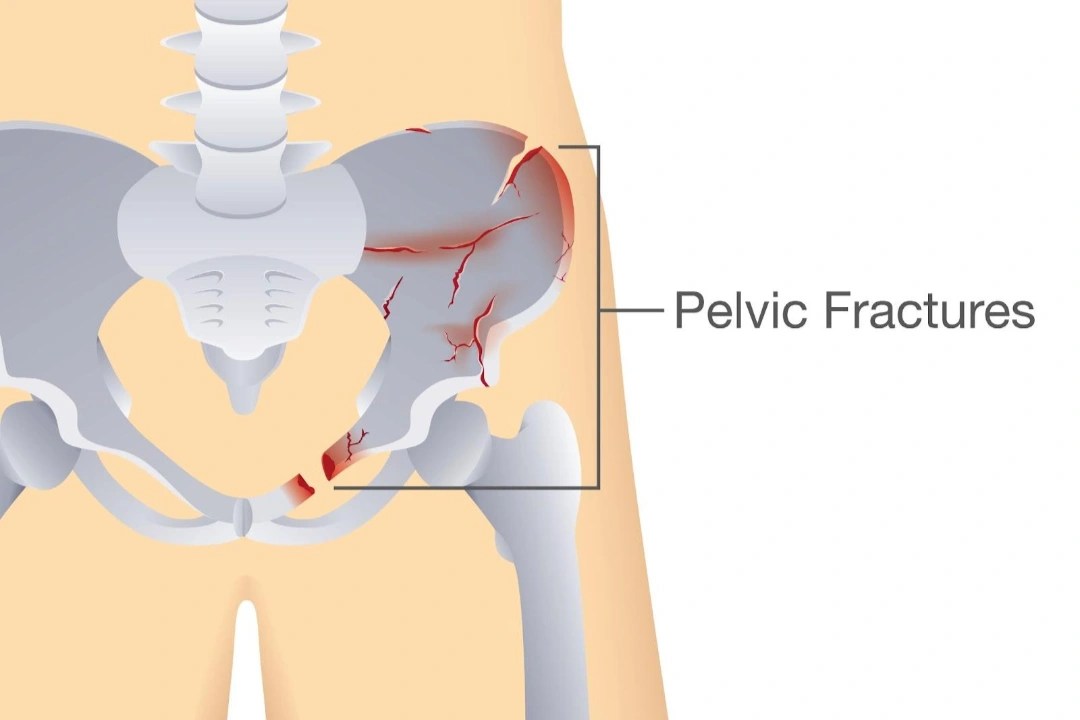
Pelvic fractures are serious injuries that can affect mobility, stability, and even internal organs depending on their severity. They may result from high-impact trauma like car accidents or from low-impact falls in individuals with weakened bones. Prompt diagnosis and appropriate management are essential to reduce complications and support recovery.

What is a pelvic fracture?
A pelvic fracture refers to a break in any of the bones that form the pelvic ring, including the ilium, ischium, pubis, sacrum, and coccyx. The pelvis plays a vital role in supporting the spine, bearing body weight, and protecting internal organs such as the bladder, intestines, and reproductive organs. When any part of this ring is broken, it is classified as a pelvic fracture. These injuries can vary in severity and are typically categorised based on the pattern and stability of the fracture.
Different types of pelvic fracture
Pelvic fractures can vary widely in their presentation and impact. They are typically grouped based on whether the skin is broken, the alignment and completeness of the break, the stability of the pelvic ring, or the involvement of muscle and ligament pull.
The table below outlines the main types of pelvic fractures, their descriptions, and what typically occurs in each case:
| Type | Description | Impact of the Fracture |
|---|---|---|
| Closed fracture | The bone is broken but the skin over the fracture remains intact. | Pain, swelling, and bruising without any visible wound. |
| Open fracture | The broken bone pierces through the skin or is exposed through a wound. | High risk of bleeding and infection; visible bone or deep wound. |
| Stable fracture | A single break with minimal displacement; the overall structure of the pelvic ring remains intact. | Localised pain with some difficulty in walking; pelvic stability is preserved. |
| Unstable fracture | Two or more breaks or dislocation of joints that disrupt the stability of the pelvic ring. | Severe pain, inability to bear weight, possible internal bleeding or injury to nearby organs. |
| Displaced fracture | The broken bone fragments have shifted out of their normal alignment. | Obvious deformity or asymmetry; more severe pain and often requires surgery. |
| Non-displaced fracture | The bone cracks but remains in correct alignment. | Localised pain and swelling; may be missed on initial X-rays without advanced imaging. |
| Complete fracture | The break goes all the way through the bone. | Sharp pain with limited mobility; often requires immobilisation or surgical fixation. |
| Partial (hairline) fracture | A crack that does not go completely through the bone. | Mild to moderate pain, especially during movement or weight-bearing; can worsen if not managed. |
| Avulsion fracture | A small piece of bone is pulled off by a tendon or ligament during a sudden muscle contraction. | Sudden, sharp pain during activity; commonly seen in athletes, especially near muscle attachments. |
What causes pelvic fractures?
Pelvic fractures can result from a variety of causes, ranging from severe accidents to weakened bone structure. The underlying cause often influences the type and severity of the fracture, as well as the treatment approach. Below are the main causes of pelvic fractures:
- High-impact trauma — this is the most common cause of pelvic fractures in younger individuals. Incidents such as road traffic accidents, falls from significant heights, or crush injuries can apply intense force to the pelvis, resulting in complex or unstable fractures. These injuries often involve multiple broken bones and may be life-threatening due to bleeding or damage to internal organs.
- Low-impact trauma — in older adults or those with osteoporosis, even minor trauma like a fall from standing height can lead to a pelvic fracture. These are known as fragility or insufficiency fractures and typically affect the pubic rami or sacrum. Age-related bone loss and poor balance increase the risk in this group.
- Sudden muscle contraction — avulsion fractures occur when a powerful or sudden muscle contraction pulls a small piece of bone away from where a tendon or ligament is attached. This type of fracture is more common in adolescents and athletes during high-intensity activities involving abrupt movements.
- Bone weakening conditions — certain diseases can weaken the bone structure, making the pelvis more vulnerable to fracture even with minimal force. These include osteoporosis, bone tumours, metastatic cancer, chronic steroid use, and metabolic bone disorders like osteomalacia or Paget’s disease.
What are the symptoms of a pelvic fracture?
The symptoms of a pelvic fracture can vary depending on the severity and type of fracture, as well as whether surrounding organs, nerves, or blood vessels are involved. While some fractures cause mild discomfort, others may produce life-threatening complications.
- Pelvic pain — pain in the hip, groin, lower back, or buttocks is often the first sign. The pain typically worsens with movement, especially when walking, standing, or trying to bear weight.
- Swelling and bruising — visible bruising, swelling, or tenderness may appear in the lower abdomen, groin, or over the bony parts of the pelvis. In some cases, bruising may extend to the genitals or thighs.
- Difficulty walking or standing — patients may find it hard or impossible to walk, stand upright, or bear weight on one or both legs. Any attempt at movement can trigger sharp pain.
- Numbness or tingling — nerve irritation or damage can lead to numbness, tingling, or weakness in the legs, buttocks, or genital area, depending on the location of the fracture.
- Urinary or bowel symptoms — pelvic fractures can sometimes injure the bladder, urethra, or bowel, leading to difficulty urinating, blood in the urine, incontinence, or abdominal bloating.
- Signs of internal bleeding — in high-impact or unstable fractures, symptoms may include dizziness, rapid pulse, low blood pressure, or signs of shock. These cases require emergency treatment.

Who is at risk of pelvic fractures in Singapore?
Pelvic fractures affect a wide range of people in Singapore, but certain groups are more vulnerable due to their age, occupation, medical conditions, or lifestyle. These groups include:
- Young males — pelvic fractures are more common in young adult males, especially those involved in road traffic accidents or falls from height. Many cases are linked to motorcycle collisions, pedestrian accidents, or construction-related injuries. These are usually high-energy trauma events that result in severe and unstable fractures.
- Older adults — with Singapore’s ageing population, elderly individuals, particularly postmenopausal women, are at higher risk due to reduced bone density. Even a minor fall at home can cause a pelvic fracture in someone with osteoporosis. Fragility fractures are expected to rise sharply in the coming years.
- People with bone-weakening conditions — individuals with chronic conditions like osteoporosis, osteomalacia, metastatic cancer, or those on long-term steroid therapy have weakened pelvic bones. In such cases, fractures can occur with minimal trauma or even routine movements like turning in bed or walking.
- Migrant workers in manual jobs — foreign labourers working in construction or industrial settings are frequently exposed to high-risk environments. Falls from scaffolding, crush injuries, or being struck by heavy objects are common causes of pelvic fractures in this group.
What are the complications of a pelvic fracture?
While some pelvic fractures heal well with appropriate care, others may lead to significant complications depending on the severity of the injury, the presence of associated damage, and how quickly treatment is provided. Complications can affect multiple systems in the body and may require ongoing medical management.
- Internal bleeding — the pelvis contains major blood vessels, and a fracture can lead to significant internal bleeding. In severe cases, this can result in hypovolaemic shock, which requires emergency intervention to stabilise the patient.
- Injury to pelvic organs — due to the close proximity of the pelvic bones to vital organs, pelvic fractures can cause tears or perforations in the bladder, urethra, rectum, or reproductive structures. This may lead to urinary retention, incontinence, or infections if not managed properly.
- Nerve damage — nerves that pass through or near the pelvis may be compressed or injured during a fracture, resulting in numbness, tingling, weakness, or difficulty controlling leg movements. In some cases, this can lead to long-term disability.
- Infection — when a fracture is open or when surgery is required to stabilise the bones, there is a risk of infection. This may involve the skin, deeper soft tissues, or even the bone itself (osteomyelitis), requiring antibiotics or further procedures.
- Chronic pain and reduced mobility — even after healing, some patients experience ongoing pelvic or lower back pain. Stiffness, gait abnormalities, or difficulty sitting for long periods may also persist, particularly in those with complex or unstable fractures.
- Deep vein thrombosis (DVT) — reduced mobility during recovery can increase the risk of blood clots forming in the legs. If a clot travels to the lungs (pulmonary embolism), it can be life-threatening. Blood-thinning medication is often given to reduce this risk.
How to prevent pelvic fractures?
Pelvic fractures can often be prevented by addressing the underlying risks, especially in vulnerable populations such as the elderly and individuals exposed to high-impact trauma. Simple steps can significantly lower the risk of trauma or bone-related fractures:
- Maintain good bone health — ensure adequate calcium and vitamin D intake and stay physically active.
- Get screened for osteoporosis — especially if you are over 50 or have risk factors for low bone density.
- Prevent household falls — use non-slip mats, secure loose rugs, and install grab bars where needed.
- Use walking aids if necessary — canes or walkers improve balance and reduce fall risk in the elderly.
- Follow workplace safety protocols — wear protective gear and use fall prevention systems in high-risk jobs.
- Be cautious during sports or exercise — warm up properly and avoid sudden, forceful movements.
- Drive safely and wear seat belts — reduces the chance of high-impact pelvic injuries in accidents.
- Manage chronic conditions — treat illnesses that affect bone strength or balance, like osteoporosis or diabetes.
How is a pelvic fracture diagnosed?
Diagnosing a pelvic fracture involves a detailed physical assessment followed by imaging tests to determine the type and extent of the fracture. In emergency settings, additional tests may be needed to identify associated internal injuries.
- Physical examination — the doctor checks for pain, swelling, bruising, deformity, limb length discrepancies, and tenderness over the pelvic bones. Signs of instability or nerve damage may also be evaluated during this stage.
- X-rays — X-rays are typically the first test ordered and can reveal breaks in the pelvic ring. They help determine if the fracture is stable or unstable, but may miss subtle or non-displaced fractures.
- CT scan — a CT (computed tomography) scan provides cross-sectional images of the pelvis and is more accurate than X-rays. It is especially useful for identifying displaced, unstable, or complex fractures that may require surgery.
- MRI scan — an MRI (magnetic resonance imaging) is occasionally used to detect occult fractures not visible on X-rays or CT, particularly in elderly patients with suspected insufficiency fractures. It can also assess injury to muscles, ligaments, and nerves.
- Urine and blood tests — these tests help identify associated injuries, such as damage to the bladder or urethra, and assess for anaemia or internal bleeding, especially in severe trauma cases.
- FAST (Focused Assessment with Sonography in Trauma) — in emergency settings, a FAST scan may be performed to quickly check for internal bleeding in the abdomen or pelvis, which is common in high-energy pelvic fractures.
What are the treatment options for a pelvic fracture in Singapore?
Treatment for pelvic fractures ranges from conservative care to surgical intervention. The approach is guided by the nature of the fracture, the patient’s overall condition, and the presence of other injuries.
- Pain management and rest — most stable fractures can be treated without surgery. Pain relief is provided through medications, and the patient is advised to limit weight-bearing activities to allow natural healing.
- Walking aids and physiotherapy — crutches, walkers, or wheelchairs may be used to help the patient move safely. Physiotherapy is started early to maintain strength, prevent stiffness, and support gradual return to walking.
- Surgical fixation — unstable pelvic fractures often need surgical intervention, such as external fixation or internal fixation using screws and plates, to stabilise the pelvic ring and restore alignment.
- Emergency stabilisation — in severe trauma cases, initial treatment may involve applying a pelvic binder, controlling internal bleeding, fluid resuscitation, or emergency surgery to stabilise the pelvis.
- Open reduction and internal fixation (ORIF) — ORIF is a surgical procedure used when the fractured pelvic bones are unstable or misaligned. The surgeon first repositions the bones (open reduction), then secures them using screws, plates, or rods (internal fixation). As it is an invasive procedure, ORIF is only performed after confirming that the patient is haemodynamically stable to minimise operative risk.
- Treatment of associated injuries — bladder, bowel, or vascular injuries are managed alongside fracture repair, often involving a multidisciplinary team to ensure comprehensive care.
Summary
Pelvic fractures are serious injuries that can result from high-impact trauma or weakened bone structure, with symptoms ranging from pelvic pain and difficulty walking to potential internal complications. Depending on the type and severity of the fracture, treatment may involve rest and physiotherapy or surgical procedures like open reduction and internal fixation. Accurate diagnosis through imaging, early intervention, and a structured rehabilitation plan are crucial to ensure optimal recovery.
If you are experiencing symptoms of a pelvic fracture or have sustained an injury that raises concern, schedule a consultation with Cove Orthopaedic Clinic for expert evaluation and personalised care.
Conditions We Treat





Frequently asked questions
How long does a pelvic fracture take to recover?
Recovery time depends on the severity of the fracture and overall health of the patient. Most stable pelvic fractures heal within 8 to 12 weeks, while more complex or surgically treated fractures may take several months, followed by rehabilitation.
Can I walk with a pelvic fracture?
In stable fractures, partial weight-bearing with crutches or a walker may be allowed under medical supervision. Unstable fractures usually require rest and non-weight-bearing until healing progresses.
What are the long-term effects of a pelvic fracture?
Some complex pelvic fractures may lead to chronic pain, altered gait, or sexual dysfunction due to nerve or muscle damage. Ongoing physiotherapy and specialist care can help improve function.
Can a pelvic fracture heal on its own?
Yes, stable pelvic fractures can often heal on their own with rest, pain management, and limited weight-bearing. However, unstable or displaced fractures usually require surgical intervention to ensure proper healing.
When should I return to sports after a pelvic fracture?
Return to activity depends on healing progress and fracture stability. It typically occurs after 12 weeks or when imaging confirms solid bone repair, guided by a physiotherapist.
What exercises can help recovery from a pelvic fracture?
Gentle range-of-motion and strengthening exercises, progressing to weight-bearing movements, aid recovery. Early physiotherapy reduces stiffness and promotes mobility.
Can pelvic fractures cause urinary issues?
Yes. Fractures may injure the bladder or urethra, leading to blood in the urine, difficulty urinating, or incontinence. This is typically assessed during diagnosis.
Can I develop blood clots after a pelvic fracture?
Yes, reduced mobility following a pelvic fracture increases the risk of deep vein thrombosis (DVT). Anticoagulant therapy is usually prescribed to prevent clots.
What is a pelvic “open-book” fracture?
An open-book fracture is an unstable injury where the pelvic ring opens like a book, commonly from front-to-back trauma. It requires urgent surgical stabilisation.



