Knee Osteoarthritis
What is Knee Osteoarthritis?
Our knees carry the brunt of our weight whenever we stand, walk, or even bend. They act as shock absorbers for the body, cushioning, cushioning the impact between our bones, providing stability and motion control.
Knee Osteoarthritis refers to the wear-and-tear of the cartilage in our knee, causing stiffness, swelling and pain over time. This often happens with age, or when we put too much stress on the knee joint, making it difficult to do simple, everyday activities such as walking or bending.

Knee osteoarthritis is a condition chracterised by pain or swelling of the knee due to wear-and-tear.
What causes Knee Osteoarthritis?
The knees are a complex joint made up of bones, cartilage, ligaments, and tendons working together to support our movement. However, like any well-used component, knee cartilage can wear down, or become damaged over time, leading to knee osteoarthritis.
This condition causes stiffness, swelling, and pain, often progressing gradually. There are certain factors that can accelerate this wear-and-tear, such as excess weight, previous knee injuries, excessive and frequent strain, and alignment issues like crooked bones or joints.
What are the common symptoms?
Some common symptoms of knee osteoarthritis include:
- Cracking or grinding noise when the knees move.
- Knees feel puffy, tender, or “stuck.”
- Loss of flexibility in the knees.
- Stiff knees, especially when you wake up in the morning or after sitting for an extended period.
- Swollen knees.
- Pain in the knees.
- Wobbly knees.
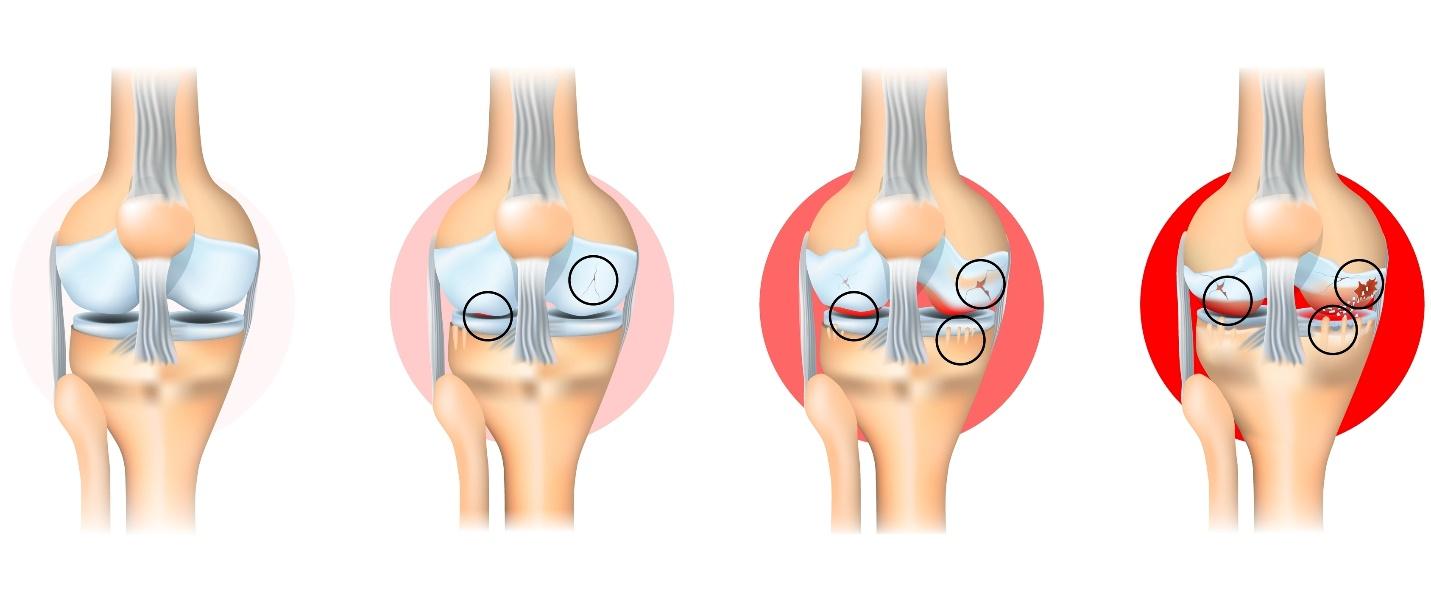
Knee osteoarthritis is categorised into four stages, depending on the severity of the condition.
What are the stages of knee osteoarthritis?
Knee osteoarthritis, when left untreated, can progress and increase in severity:
- Stage 1 (minor) — Early wear-and-tear with little pain or discomfort. Some bone growths may form around the joint, but this typically doesn’t affect movement.
- Stage 2 (mild) — Stiffness after sitting or performing certain movements that involve the knees. Cartilage slowly starts to break down during this stage.
- Stage 3 (moderate) — Cartilage damage worsens and bone growths become more significant. Joint stiffness and pain increase as the space between the joints narrow, causing pain and discomfort.
- Stage 4 (severe) — Cartilage is almost entirely worn away, causing severe pain, inflammation, stiffness, and difficulty moving the knee.
Who is at risk of developing Knee Osteoarthritis in Singapore?
Knee osteoarthritis affects approximately 46% of people. However, there are certain groups of people who are more susceptible to developing the condition. This includes:
- Age — individuals who are 40 years old and older are more likely to develop knee osteoarthritis due to the natural ageing process.
- Gender — women are at a higher risk of developing knee osteoarthritis compared to men. This is because anatomically, women have wider hips and knock-kneed, leading to more stress on the knee joints and causing them to tilt inwards.
- Genetics — individuals with a family history of knee osteoarthritis have a 40% possibility of developing the condition. In fact, genetics accounts for roughly 35% to 65% of all knee osteoarthritis cases.
- Knee injuries — certain injuries, such as meniscal tears and anterior cruciate ligament (ACL) ruptures, can increase the likelihood of developing knee osteoarthritis by 25% to 50%.
How is Knee Osteoarthritis diagnosed in Singapore?
Diagnosing knee osteoarthritis is a straightforward procedure that entails a series of examinations. At Cove Orthopaedic, our Orthopaedic Specialist begins the consultation by performing a physical examination.
During a physical examination, our orthopaedic specialist will conduct the following assessments to measure your range of motion, and severity of the pain:
- To identify if your knees are sore, or red.
- To identify potential injuries to the knees.
- To identify your knees’ range of motion.
- To identify the severity of your knee pain.
Aside from a physical examination, our orthopaedic specialist may also insist on having the following test performed to facilitate the diagnostic process.
- Blood tests – blood tests are typically conducted to rule out other causes of joint pain, such as rheumatoid arthritis or other inflammatory conditions. While blood tests do not directly diagnose osteoarthritis, they help eliminate other potential causes of knee pain.
- Joint aspiration – joint aspiration, better known as arthrocentesis, involves drawing fluids from the knee joint with a needle. The fluid is then analysed to check for signs of infection, inflammation, or crystal deposits, which can help differentiate osteoarthritis from other joint conditions, such as gout or septic arthritis.
Our orthopaedic specialist may also order one or a combination of imaging tests to be performed, such as:
- Magnetic resonance imagery (MRI) – an MRI scan provides detailed images of both bone, and soft tissue structures of the knees. It allows our orthopaedic specialist to assess damages to the cartilage, ligaments, and tendons around the knees, as well as identify potential inflammation or structural changes in the joint.
- X-ray – X-rays are commonly used as an initial imaging tool to evaluate knee osteoarthritis. They help detect narrowing of the joint space, bone spurs, and other changes in the bone structure that are characteristic of osteoarthritis.

How is Knee Osteoarthritis treated in Singapore?
Treatment for knee osteoarthritis will depend on several factors, such as the severity of the condition, and age. While both non-surgical, and surgical treatment options are available, this will depend on how progressive the condition is.
Conservative Treatments
Early stages of knee osteoarthritis often respond well to non-surgical treatment options, such as:
- Knee brace – wearing a supporting knee brace can stabilise the knee joint, and help alleviate pain, making daily movements more manageable.
- Lifestyle changes – simple lifestyle adjustments, such as reducing high-impact activities, and maintaining a healthy weight, can help alleviate symptoms. Similarly, it will help in reducing stress on the knee joints.
- Injections – corticosteroid, or hyaluronic acid injections may be recommended for temporary pain relief, and to reduce inflammation in the knee joint.
- Medication – non-steroidal anti-inflammatory drugs (NSAIDs), or acetaminophen are commonly prescribed to relieve pain, and reduce inflammation associated with osteoarthritis.
- Physical therapy – physical therapy focuses on strengthening the muscles around the knee, improving flexibility, and enhancing joint stability, which can significantly reduce pain, and improve mobility.
Surgical Treatments
For advanced cases, surgery may be recommended to relieve pain, and restore joint function. This includes:
- Arthroscopy – for mild to moderate cases, arthroscopy may be performed to remove loose cartilage fragments, or smooth out rough surfaces, providing temporary relief from pain, and inflammation.
- Osteotomy – osteotomy involves cutting, and reshaping bones to reduce the load on the damaged part of the knee, helping to preserve the joint, and relieve pain.
- Partial or Total knee replacement – in more severe cases, partial or total knee replacement may be performed to replace the damaged knee joint with artificial components, significantly improving mobility, and quality of life.
Rehabilitation Process
A structured, and personalised rehabilitation plan is often outlined to complement treatment procedures. This is essential, as it helps to ensure that the knees are recovering optimally. Depending on your condition, our orthopaedic specialist may recommend the following rehabilitative measures:
- Assistive devices – crutches, or a walker may be used initially to offload weight from the knee during the early stages of recovery.
- Range of motion (ROM) – ROM exercises are designed to help maintain joint flexibility, and prevent stiffness. This is crucial for post-operative recovery, and long-term function.
- Strength training – strengthening exercises focus on building the quadriceps, hamstrings, and other muscles supporting the knee to enhance joint stability.
- Weight-bearing progression – patients who underwent surgical treatments will begin with weight-bearing exercises, and progress gradually to full weight-bearing to rebuild strength, and stability.

If you have been experiencing knee pain, or have a risk of developing knee osteoarthritis, then we urge you to schedule a consultation (link to contact page). By getting an early diagnosis, you will have access to immediate treatment that will improve your treatment outcomes, simultaneously preserving your quality of life.
Frequently Asked Questions
What happens if Knee Osteoarthritis is left untreated?
If left untreated, knee osteoarthritis can worsen, leading to increased pain, joint stiffness, and swelling. Over time, it may severely limit mobility, making it difficult to perform basic day-to-day tasks like walking, climbing the stairs, or standing for long periods.
Additionally, untreated knee osteoarthritis can also cause the joint to deform as the cartilage continues to wear down, resulting in increased strain on surrounding muscles, and other joints. This can potentially cause further complications, and deteriorate your quality of life.
How does having Knee Osteoarthritis affect my quality of life?
Knee osteoarthritis significantly impacts your quality of life, particularly through chronic pain, and reduced mobility. Many people have trouble with activities they once enjoyed, like exercising, going for long walks. This eventually affects both their physical, and mental health are reduced activity can lead to weight gain, muscle weakness, and feelings of frustration or depression due to limited independence.
Why is it important for me to see an orthopaedic specialist instead of a general practitioner for Knee Osteoarthritis?
An orthopaedic specialist has advanced training specifically in joint conditions, and can offer specialised care, including more precise diagnosis, and targeted treatment options like physical therapy, injections, or surgery if needed.
This specialist insight is crucial for tailoring a treatment plan that addresses both the current symptoms, and long-term joint health.
What are the chances of Knee Osteoarthritis recurring after treatment?
While treatment can alleviate symptoms, and improve joint function, knee osteoarthritis is a chronic condition. Many treatments, such as medications or injections, provide temporary relief, and symptoms may recur as the joint continues to age, or if there is repeated stress, or injury.
On the other hand, surgical interventions, like knee replacement, have longer-lasting effects, but it is still important to follow a tailored physical therapy, or exercise programme to help maintain results, and reduce the likelihood of recurrence.
Is it possible to prevent Knee Osteoarthritis?
Unfortunately, knee osteoarthritis is not a preventable condition. However, there are ways to lower your risk factor, such as:
- Avoiding excessive weight gain.
- Maintaining a healthy weight to reduce joint strain.
- Staying physically active to strengthen surrounding muscles.











