Patella
Tendinopathy
- Home
- Conditions We Treat
- Knee
- Patella Tendinopathy
What is Patella Tendinopathy?
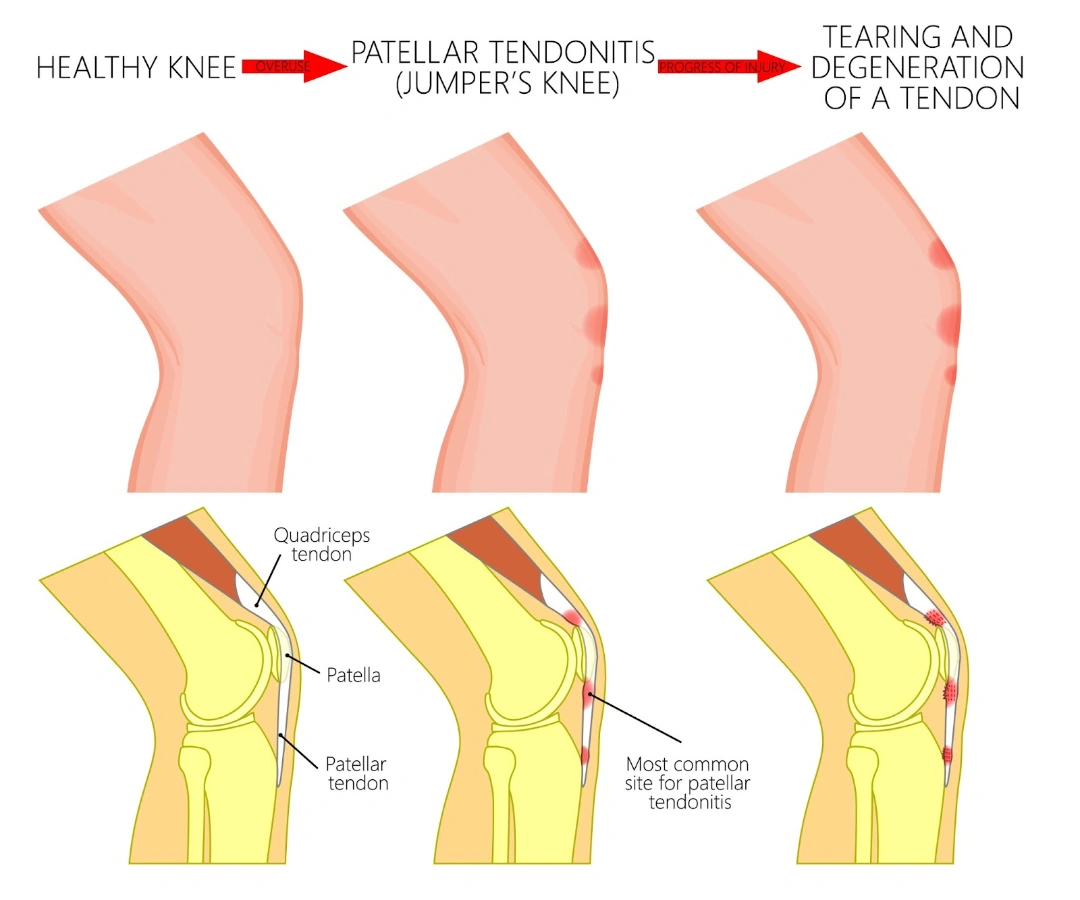
Patella tendinopathy, also known as “jumper’s knee,” is a condition affecting the patellar tendon, which connects the kneecap (patella) to the shinbone (tibia). This tendon plays a vital role in extending the knee, allowing for movements like jumping, running, and kicking. In patella tendinopathy, the tendon undergoes wear and tear due to repetitive stress or overuse, often from high-impact activities.
This condition is characterised by pain and inflammation at the lower part of the kneecap, specifically where the tendon attaches. Over time, these repetitive movements can lead to tendon degeneration, resulting in persistent discomfort and difficulty with knee function.
What causes Patella Tendinopathy?
Excessive stress on the patellar tendon
Patella tendinopathy develops from repetitive stress placed on the patellar tendon, which results in a gradual breakdown of the tendon fibres over time. This condition is primarily caused by a cycle of microtears in the tendon that occur with repeated loading, particularly during activities that involve forceful knee extension, like jumping or abrupt changes in movement. When the knee is overworked, the tendon fibres are strained beyond their capacity, leading to microscopic damage that can accumulate without adequate recovery.
Tendon degeneration
The underlying mechanism involves a process called “tendon degeneration.” Unlike a typical inflammatory response seen in acute injuries, patella tendinopathy is often associated with a failure of the tendon to repair itself fully. The damaged fibres don’t heal as normal tissue but instead begin to degenerate, resulting in structural changes within the tendon. Over time, the healthy, organised collagen fibres in the tendon are replaced with disorganised tissue, which weakens the tendon and reduces its elasticity.
Disrupted blood flow within the tendon
Another contributing factor to this degenerative process is the disruption of blood flow within the tendon. Tendons naturally receive a lower blood supply than muscles, which limits their capacity for healing. Repeated stress on the patellar tendon further restricts blood flow, which hinders the delivery of oxygen and nutrients essential for tissue repair. This limited healing environment can prolong the degenerative changes in the tendon, making recovery more challenging.
What are the symptoms of Patella Tendinopathy?
Patella tendinopathy typically presents with a distinct set of symptoms focused around the knee. Individuals with this condition may experience the following:
- Pain below the kneecap — Pain localised just below the kneecap, especially noticeable during activities involving knee movement.
- Tenderness and sensitivity — Tenderness and sensitivity to touch at the lower part of the patella.
- Stiffness — Stiffness in the knee, particularly after periods of inactivity, such as sitting or sleeping.
- Pain during physical activities — Increased pain during physical activities, especially those that involve jumping, running, or climbing stairs.
- Weakness or instability — A sensation of weakness or instability in the knee when performing weight-bearing movements.

Who is at risk for Patella Tendinopathy in Singapore?
Patella tendinopathy can affect anyone, but certain groups are more susceptible due to lifestyle factors, activity levels, and physical demands. In Singapore, those most at risk include:
- Athletes in high-impact sports — individuals involved in sports like basketball, volleyball, and soccer, which require frequent jumping and abrupt changes in direction.
- Recreational runners — running enthusiasts who may not always have consistent training routines or proper recovery periods.
- Individuals with sedentary jobs — people who spend long hours sitting may have weakened quadriceps and hamstrings, increasing strain on the patellar tendon when active.
- Fitness enthusiasts — individuals participating in high-intensity interval training (HIIT) or strength training, especially with poor form or rapid increases in workout intensity.
- Older adults engaged in physical activity — age-related changes in tendon elasticity make this group more vulnerable when participating in high-impact or repetitive activities.
- Individuals with previous knee injuries — those with a history of knee injuries, such as ligament tears or fractures, which may predispose the tendon to overuse and damage.
How is Patella Tendinopathy diagnosed?
At Cove Orthopaedic Clinic, we prioritise a thorough and accurate diagnosis to ensure the best treatment path for patella tendinopathy. We use a range of methods to evaluate your knee condition and pinpoint the cause of your discomfort:
- Detailed physical examination — our specialists carefully assess the knee for tenderness, pain, and functional limitations, often performing specific movements to identify patellar tendon involvement.
- Patient’s history — we take the time to discuss your activity levels, recent changes in physical routines, and any previous knee injuries that could contribute to the issue.
- Ultrasound imaging: this non-invasive imaging technique allows us to visualise the patellar tendon and detect any degeneration or microtears in the tendon fibres.
- Magnetic Resonance Imaging (MRI) — in cases where more detailed imaging is needed, an MRI provides a comprehensive view of the tendon structure and can reveal any advanced degenerative changes.
With these diagnostic tools, the healthcare team at Cove Orthopaedics ensures a clear understanding of your knee’s condition that can help tailor a treatment plan that’s right for you.
What are the treatment options for Patella Tendinopathy in Singapore?
Our approach combines specialised techniques and personalised care to address each patient’s unique needs:
- Activity modification and rest — we guide you on adjusting physical activities to reduce strain on the patellar tendon, which can give it the chance to heal while maintaining overall fitness.
- Physical therapy — our therapists design a personalised programme focusing on strengthening and stretching exercises for the quadriceps, hamstrings, and calf muscles to restore balance and support the knee.
- Shockwave therapy — this non-invasive treatment uses acoustic waves to stimulate healing in the affected tendon, promoting tissue regeneration and pain relief.
- Platelet-Rich Plasma (PRP) injections — for cases requiring enhanced healing, we may use PRP injections, which harness growth factors from your blood to stimulate tendon repair.
- Patellar taping or bracing — we offer supportive taping or bracing options to alleviate stress on the tendon and help stabilise the knee during movement.
- Ultrasound-Guided Dry Needling — in select cases, dry needling can encourage healing within the tendon by promoting blood flow and breaking down scar tissue.
- Surgical intervention — for severe or persistent cases, minimally invasive surgery may be an option, where we carefully remove damaged tissue to support healthier tendon function.
At Cove Orthopaedic Clinic, our goal is to provide a comprehensive approach to managing patella tendinopathy, helping you achieve long-lasting relief and return to your activities with confidence.
If you’re experiencing persistent knee pain or discomfort below the kneecap, schedule a consultation (link to ‘Contact Us’ page) with us for a thorough evaluation and personalised treatment plan to help you get back to your active lifestyle.
Conditions We Treat





Frequently asked questions
Can patella tendinopathy heal on its own?
Patella tendinopathy may improve with rest and activity modification; however, without appropriate treatment, it can become chronic. Engaging in targeted physical therapy and following a structured rehabilitation program are crucial for effective recovery.
How long does it take to recover from patella tendinopathy?
Recovery time varies depending on the severity of the condition and adherence to treatment protocols. Mild cases may resolve within a few weeks, while more severe instances can take several months to heal fully.
Is it safe to exercise with patella tendinopathy?
Engaging in low-impact exercises that do not exacerbate pain is generally safe and can aid recovery. It’s essential to avoid activities that strain the patellar tendon and to consult a healthcare professional for a tailored exercise plan.
What are the best exercises for patella tendinopathy?
Eccentric strengthening exercises, such as decline squats, are beneficial for patella tendinopathy. Additionally, stretching the quadriceps and hamstrings can help alleviate tension on the tendon. Always perform exercises under professional guidance to ensure proper technique.
Can patella tendinopathy lead to other complications?
If left untreated, patella tendinopathy can progress, leading to tendon degeneration and, in rare cases, tendon rupture. Early intervention is key to preventing such complications.
Are there preventive measures for patella tendinopathy?
Yes, maintaining strong and flexible leg muscles, using proper techniques during physical activities, and gradually increasing activity intensity can help prevent patella tendinopathy. Wearing appropriate footwear and avoiding sudden changes in training routines are also beneficial.
Is patella tendinopathy the same as patellofemoral pain syndrome?
No, while both conditions cause anterior knee pain, they differ in origin. Patella tendinopathy involves the patellar tendon, whereas patellofemoral pain syndrome relates to issues between the kneecap and the femur.
When should I see a doctor for patella tendinopathy?
If you experience persistent knee pain that doesn’t improve with rest, or if the pain interferes with daily activities, it’s advisable to consult a healthcare professional for a comprehensive evaluation and appropriate treatment plan.



