Tendinitis (Tendon Inflammation)
What is tendinitis (tendon inflammation)?
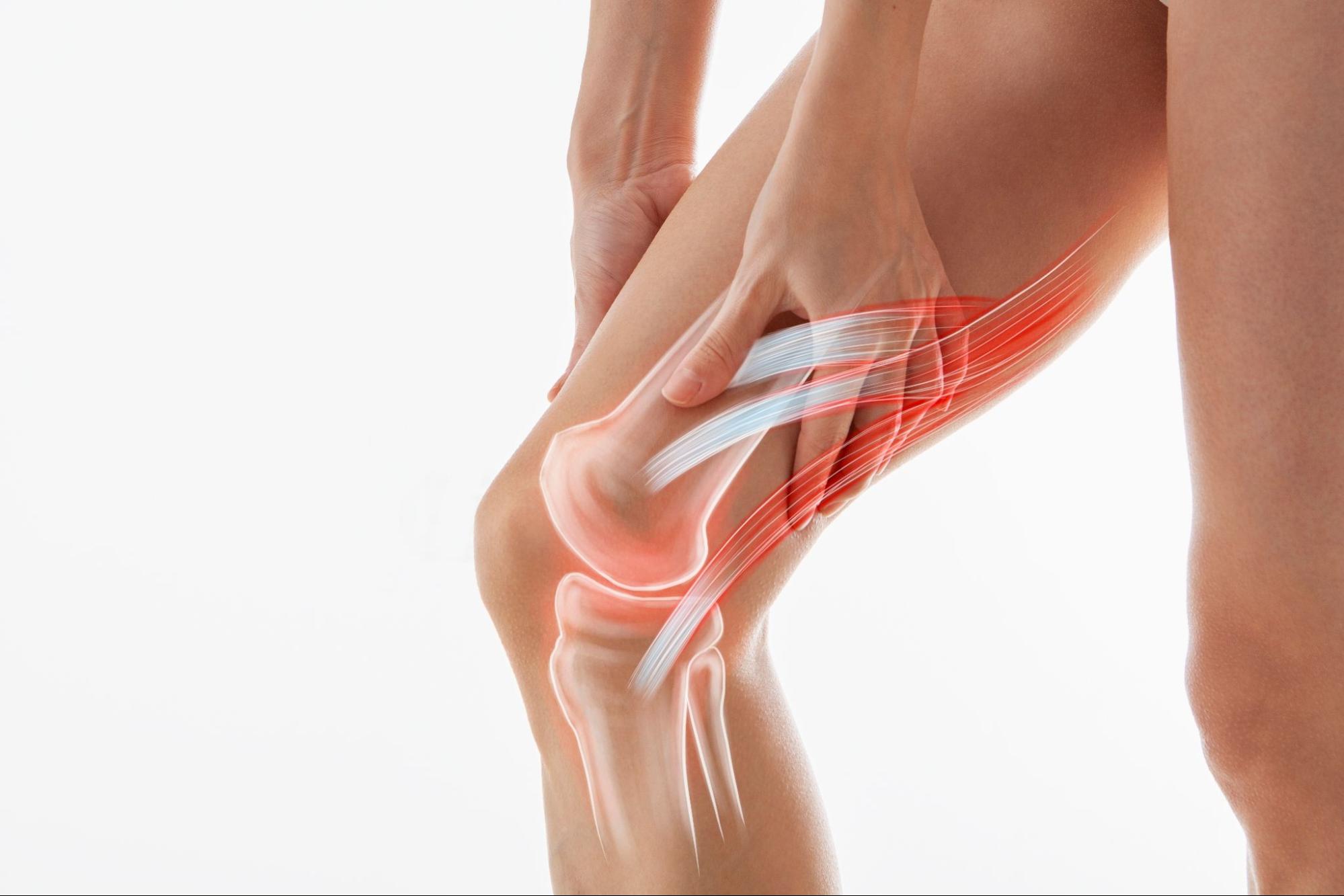
Tendinitis, also known as tendon inflammation, refers to the irritation or swelling of a tendon — a thick, fibrous structure that connects muscle to bone. This condition typically develops due to repetitive movements, excessive strain, or sudden injuries that overstress the tendon. It can cause localised pain, tenderness, and restricted movement in the affected area.
Tendons are strong fibrous bands designed to withstand tension, but when subjected to excessive or repetitive force without adequate recovery, microscopic tears can develop within the fibres. Over time, these tears can lead to inflammation, resulting in pain and discomfort. While tendinitis can occur in any tendon, it is most common in areas subject to frequent motion, such as the shoulders, elbows, wrists, knees, and heels.
The severity of tendinitis varies from mild irritation to more persistent pain that limits daily activities. If left untreated, it may lead to chronic tendon degeneration, known as tendinosis, which can weaken the tendon and increase the risk of rupture.
Patellar tendinitis, also known as jumper’s knee, is the inflammation of the patellar tendon, causing pain below the kneecap and often affecting athletes in jumping sports.
Common types of tendinitis
Tendinitis can occur in any tendon, but certain areas of the body are more prone to inflammation due to repetitive use or mechanical stress. Understanding the common types of tendinitis helps in early recognition and targeted treatment.
- Rotator cuff tendinitis — affects the tendons around the shoulder joint. This type involves inflammation of the tendons in the rotator cuff, a group of muscles and tendons that stabilise the shoulder. It is common among swimmers, painters, and those who perform overhead activities. Symptoms include shoulder pain when lifting the arm or lying on the affected side.
- Lateral epicondylitis — also known as tennis elbow. Despite the name, tennis elbow is not exclusive to athletes. It results from repetitive wrist and arm movements that stress the tendons on the outer part of the elbow. Common symptoms include pain when gripping objects or extending the forearm.
- Medial epicondylitis — commonly referred to as golfer’s elbow. This condition affects the tendons on the inner side of the elbow and is associated with repetitive forearm use. People who frequently lift, throw, or swing may develop this condition. Pain typically worsens with gripping or wrist flexion.
- Achilles tendinitis — inflammation of the Achilles tendon at the back of the heel. Often seen in runners or individuals who suddenly increase physical activity, this type causes pain and stiffness along the back of the leg near the heel. It may feel worse in the morning or after prolonged rest.
- Patellar tendinitis — also called jumper’s knee. This form of tendinitis involves the tendon connecting the kneecap to the shinbone and is common in sports involving jumping or running. Pain is typically felt just below the kneecap and worsens with activity, particularly jumping or climbing stairs.
- De Quervain’s tenosynovitis — inflammation of tendons on the thumb side of the wrist. This type affects the tendons running along the base of the thumb, causing pain during gripping, pinching, or twisting motions. It is often seen in new mothers, individuals with repetitive wrist movements, or those who frequently lift infants or groceries.
What causes tendinitis?
Tendinitis occurs when excessive strain on a tendon leads to microscopic damage and an inflammatory response. Tendons are composed primarily of collagen fibres arranged in a parallel structure to withstand tension and facilitate smooth movement between muscles and bones.
- Stress, overuse or sudden force — However, when subjected to repetitive stress, overuse, or sudden force, the tendon’s ability to repair itself becomes compromised. This results in collagen breakdown, swelling, and pain, which characterise tendinitis.
- Poor blood circulation — Another key factor in the development of tendinitis is the role of vascular supply. Tendons have a relatively low blood supply compared to muscles, which limits their ability to receive oxygen and nutrients necessary for rapid healing. Areas of tendons with particularly poor circulation, such as the Achilles tendon or rotator cuff tendons, are more prone to degenerative changes when exposed to ongoing mechanical stress. Inflammatory cells and biochemical mediators, including cytokines and prostaglandins, contribute to further tissue irritation and pain.
If the tendon remains under excessive strain without proper management, inflammation may give way to degenerative changes, a process known as tendinosis. Unlike acute tendinitis, tendinosis involves the progressive breakdown of tendon fibres without significant inflammatory cell infiltration.

Patellar tendinitis (jumper’s knee) is caused by repetitive stress on the patellar tendon, often from jumping, running, or sudden increases in physical activity, leading to microtears and inflammation.
What are the symptoms of tendinitis?
Tendinitis typically presents with pain and discomfort in the affected tendon, often worsening with movement or activity. The severity of symptoms can vary depending on the extent of tendon involvement and the duration of the condition. Common symptoms include:
- Pain and tenderness – localised pain that may be sharp during movement and dull or aching at rest.
- Swelling – mild to moderate swelling around the affected tendon due to inflammation.
- Stiffness and reduced mobility – difficulty moving the affected joint, especially after periods of inactivity.
- Warmth and redness – the inflamed area may feel warm to the touch and, in some cases, appear reddened.
- Crepitus (grating sensation) – a crackling or grating feeling when moving the tendon, often accompanied by mild discomfort.
- Pain that worsens with activity – symptoms typically intensify with repetitive movements or increased physical exertion.
- Weakness in the affected area – reduced strength in the associated muscle due to pain and inflammation.
Symptoms often develop gradually but can become persistent if the underlying strain is not addressed. Early recognition and appropriate management can help prevent progression to chronic tendon damage.
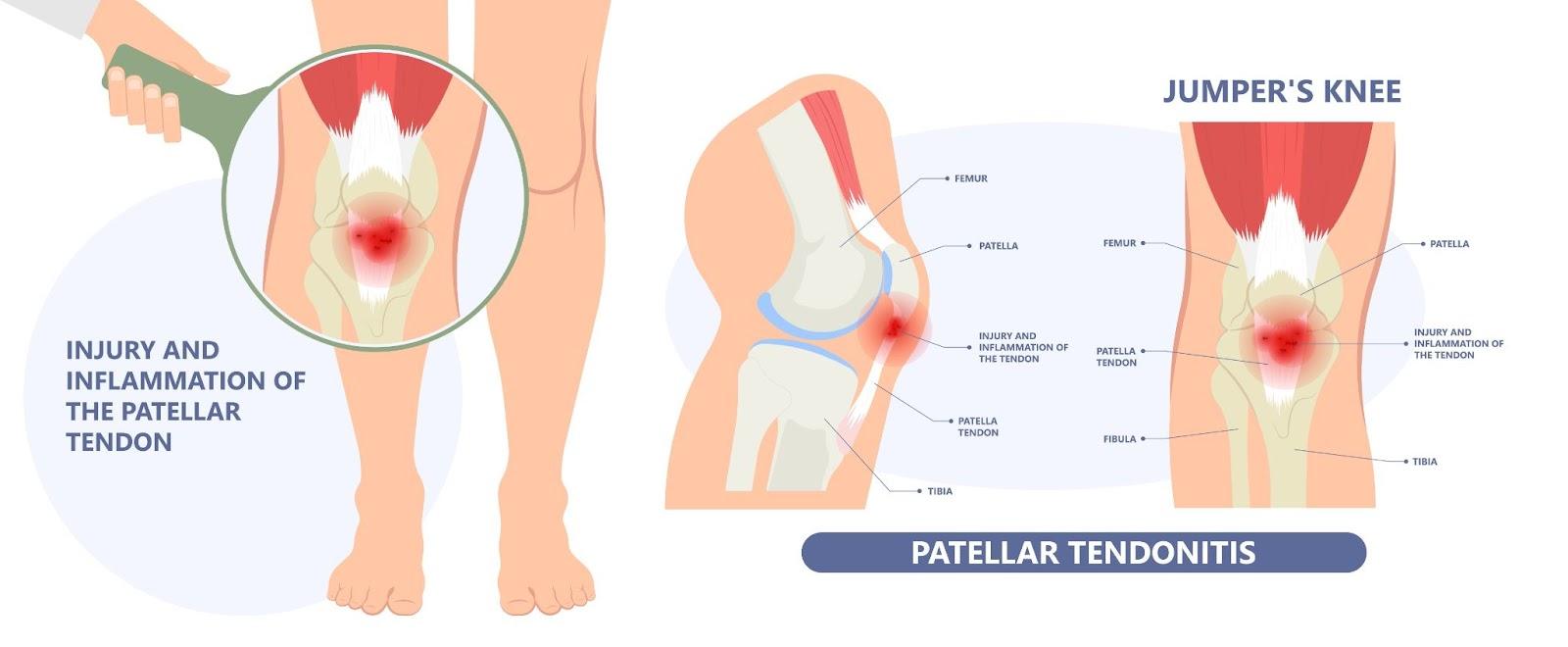
Tendinitis, such as patellar tendinitis (jumper’s knee) causes pain and tenderness just below the kneecap, especially during movement or pressure on the tendon.
Who is at risk of tendinitis in Singapore?
Tendinitis can affect individuals across various age groups and activity levels, but certain factors increase the likelihood of developing the condition. In Singapore, where a fast-paced lifestyle, high participation in sports, and extended working hours are common, specific groups are more prone to tendon inflammation. Key risk factors include:
- Office workers – repetitive typing and mouse use may strain wrist and forearm tendons.
- Athletes – high-impact sports like tennis, badminton, and running stress the tendons.
- Construction and manual labourers – heavy lifting and repetitive motions overload tendons.
- Older adults – tendons lose elasticity with age, making them more prone to injury.
- Musicians and artists – fine motor movements can overwork hand and arm tendons.
- Healthcare professionals – frequent bending, lifting, and fine movements increase strain.
- People with poor posture – incorrect posture puts extra pressure on certain tendons.
- Those with underlying conditions – diabetes, rheumatoid arthritis, and gout affect tendon health.
How is tendinitis diagnosed?
At Cove Orthopaedics, we take a thorough and personalised approach to diagnosing tendinitis to ensure that each patient receives an accurate assessment and appropriate treatment plan. Our specialists use a combination of clinical evaluation and comprehensive imaging techniques to confirm the condition and rule out other potential causes of tendon pain. Diagnostic methods include:
- Comprehensive medical history and physical examination – we begin by understanding your symptoms, activity levels, and any previous injuries. A physical assessment helps identify tenderness, swelling, and range of motion limitations.
- Ultrasound imaging – high-resolution ultrasound allows us to visualise tendon structure in real-time, which helps us detect inflammation, tears, or thickening of the tendon.
- Magnetic Resonance Imaging (MRI) – in cases where deeper tissue assessment is required, an MRI provides detailed images of the tendon and surrounding structures, which helps us differentiate between tendinitis and other conditions like tendinosis or partial tears.
- X-rays (to rule out other conditions) – while tendinitis itself is not visible on X-rays, this imaging method helps exclude bone-related issues such as calcifications or joint abnormalities that may contribute to pain.
What are the treatment options for tendinitis in Singapore?
Depending on the severity of tendinitis, treatment may include:
- Activity modification and rest – we guide patients on adjusting their activities to reduce stress on the affected tendon while maintaining overall mobility.
- Physiotherapy and rehabilitation – our specialists work closely with physiotherapists to develop personalised exercise programmes that improve flexibility, strengthen surrounding muscles, and enhance tendon recovery.
- Medications for pain and inflammation – non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended to alleviate pain and swelling in acute cases.
- Shockwave therapy – this non-invasive treatment stimulates blood flow and promotes tissue healing, which makes it particularly effective for chronic tendinitis.
- Ultrasound-guided corticosteroid injections – for persistent inflammation, targeted steroid injections provide temporary relief by reducing swelling and pain in the affected tendon.
- Platelet-rich plasma (PRP) therapy – we offer regenerative treatments like PRP therapy, where concentrated growth factors from the patient’s blood are injected into the tendon to accelerate healing.
- Bracing and orthotic support – custom braces, splints, or shoe inserts may be recommended to offload stress from the tendon and support proper movement.
- Surgical intervention (for severe cases) – in rare cases where tendinitis has progressed to significant tendon damage, minimally invasive surgery may be considered to remove damaged tissue and stimulate healing.
Summary
If you are struggling with persistent tendon pain or limited mobility, schedule a consultation with us for a thorough diagnosis and personalised treatment plan to restore your movement and comfort.
Frequently Asked Questions (FAQ)
Can tendinitis heal on its own?
Mild cases of tendinitis may resolve with rest, activity modification, and home care measures. However, without proper management, tendinitis can persist or worsen, potentially leading to chronic issues. It’s advisable to consult a healthcare professional for appropriate guidance.
Is it advisable to exercise with tendinitis?
Engaging in activities that exacerbate tendinitis symptoms can impede healing. However, specific exercises, particularly those focusing on gentle stretching and strengthening, may aid recovery. A physiotherapist can develop a personalised exercise programme to facilitate healing without overloading the tendon.
When should I seek medical attention for tendinitis?
If you experience persistent pain, swelling, or stiffness that does not improve with rest and home care, or if symptoms worsen, it’s important to consult a healthcare provider. Early intervention can prevent further tendon damage and promote effective recovery.
Can tendinitis recur after treatment?
Yes, tendinitis can recur, especially if the underlying causes, such as repetitive strain or improper technique, are not addressed. Implementing preventive measures, including proper ergonomics, regular stretching, and strength training, can reduce the risk of recurrence.
Are there any long-term complications associated with untreated tendinitis?
If left untreated, tendinitis can lead to tendon degeneration, known as tendinosis, which weakens the tendon and increases the risk of rupture. Chronic pain and reduced joint mobility are also potential complications. Timely treatment is essential to prevent these outcomes.











